News
New Studies Suggest Vaping Could Cloud Your Thoughts
Monday, December 28, 2020
Two new studies from the University of Rochester Medical Center (URMC) have uncovered an association between vaping and mental fog. Both adults and kids who vape were more likely to report difficulty concentrating, remembering, or making decisions than their non-vaping, non-smoking peers. It also appeared that kids were more likely to experience mental fog if they started vaping before the age of 14.
While other studies have found an association between vaping and mental impairment in animals, the URMC team is the first to draw this connection in people. Led by Dongmei Li, Ph.D., associate professor in the Clinical and Translational Science Institute at URMC, the team mined data from two major national surveys.
"Our studies add to growing evidence that vaping should not be considered a safe alternative to tobacco smoking," said study author Li.
The studies, published in the journals Tobacco Induced Diseases and Plos One, analyzed over 18,000 middle and high school student responses to the National Youth Tobacco Survey and more than 886,000 responses to the Behavioral Risk Factor Surveillance System phone survey from U.S. adults. Both surveys ask similar questions about smoking and vaping habits as well as issues with mental function.
Both studies show that people who smoke and vape -- regardless of age -- were most likely to report struggling with mental function. Behind that group, people who only vape or only smoke reported mental fog at similar rates, which were significantly higher than those reported by people who don't smoke or vape.
The youth study also found that students who reported starting to vape early -- between eight and 13 years of age -- were more likely to report difficulty concentrating, remembering, or making decisions than those who started vaping at 14 or older.
"With the recent rise in teen vaping, this is very concerning and suggests that we need to intervene even earlier," said Li. "Prevention programs that start in middle or high school might actually be too late."
Adolescence is a critical period for brain development, especially for higher-order mental function, which means tweens and teens may be more susceptible to nicotine-induced brain changes. While e-cigarettes lack many of the dangerous compounds found in tobacco cigarettes, they deliver the same amount - or possibly more - nicotine.
While the URMC studies clearly show an association between vaping and mental function, it's not clear which causes which. It is possible that nicotine exposure through vaping causes difficulty with mental function. But it is equally possible that people who report mental fog are simply more likely to smoke or vape -- possibly to self-medicate.
Li and her team say that further studies that follow kids and adults over time are needed to parse the cause and effect of vaping and mental fog.
In addition to Li, authors of the youth study include Catherine Xie, and Zidian Xie, Ph.D. For the adult study, Li was joined by co-authors Zidian Xie, Ph.D., Deborah J. Ossip, Ph.D. Irfan Rahman, Ph.D., and Richard J. O'Connor, Ph.D. Both studies were funded by the National Cancer Institute and the U.S. Food and Drug Administration's Center for Tobacco Products.
Researchers Find Nationwide Links Between Vaping and COVID-19
Wednesday, December 2, 2020
States with more vapers had larger numbers of daily coronavirus cases and deaths in the early weeks of the pandemic — with New York state as a hot spot, according to an analysis by the University of Rochester Medical Center.
Led by Dongmei Li, Ph.D., an expert in biostatistics at URMC, the study adds to growing national data that links vaping and the coronavirus. Although the current analysis does not provide a direct cause-and-effect between the two, it raises more concerns about vaping, which has also been linked to outbreaks of other illnesses and deaths from the chemicals in vaping products.
The journal Preventive Medicine Reportspublished Li's findings.
"As the country comes to grips with behaviors that may raise or lower risks of contracting COVID-19," Li said, "our study supports the possibility that vaping increases the risk."
Li and her team analyzed integrated population data in each U.S. state from the Centers for Disease Control and Prevention (CDC) 2018 Behavioral Risk Factor Surveillance System (BRFSS). The BRFSS annually surveys about 400,000 Americans on health habits and risks. For this project, researchers focused on vaping data. They also gathered coronavirus cases and deaths from CDC data and other reliable sources, and then used statistical models to examine the prevalence of e-cigarette use and coronavirus infections from Jan. 21, 2020 to April 25, 2020.
The study also found that less education played a role in the number of infections. States with a higher proportion of residents without a high school degree, for example, had higher coronavirus death rates.
Seminar on aerosol transmission of COVID-19
Wednesday, November 18, 2020
This seminar was presented on November 18th as part of the Epidemiology Seminar Series. Dr. Hopke provided an introduction to the nature of particles, particle sizes, and particle behavior in the atmosphere and the respiratory tract, including a discussion of the evidence for aerosol transmission of COVID-19.
Special Department of Microbiology and Immunology Seminar – Dr. Malika Grayson – November 9th at NOON
Friday, October 23, 2020
How do you make an impact when you are the only person in the room that looks like you? We hear the terms diversity and inclusion but forget that the term representation should be a reflection of diversity and inclusion combined. This isn't always the case. Dr. Grayson discusses her views on what it means to increase diversity and representation as an Individual Contributor. Learn more about her journey as the 2nd Black Woman to graduate with a PhD in Mechanical Engineering from her graduate institution. Hear about her current work as both an engineer, a STEM Advocate, and her most recent success as author of 'HOODED: A Black Girl's Guide to the PhD' where she highlights her time and lessons learned during her PhD Program.

University joins 21-Day Racial Equity Challenge
Thursday, October 22, 2020
To deepen our understanding of how racism and inequity affect our lives and our community, the University has joined the United Way's 21-Day Racial Equity Challenge, October 23--November 20. "An important part of dismantling racism is understanding the pervasive forces of bigotry and bias," says Mercedes Ramírez Fernández, the Richard Feldman Vice President for Equity and Inclusion and chief diversity officer. "The more we openly and honestly address these issues as a community, the more we create a welcoming, respectful, and safe environment where everyone can study, work, and live. I encourage everyone to participate in the 21-Day Equity Challenge and I look forward to the many ways it will inspire our continuing work for greater equity, diversity, and inclusion."
Cross-Sector Partnerships Help Underrepresented Communities SARS-COV-2 Crisis
Tuesday, October 20, 2020
Academic medical centers must establish cross-sector and cross-discipline community partnerships, and these partnerships are critical for effective crisis response in lieu of the COVID pandemic, according to a new paper published in the Journal of American Medical Association by authors from the Department of Pediatrics at the University of Rochester Medical Center (URMC).
The paper, "Leveraging Cross-Sector Partnerships to Preserve Child Health: A Call to Action in a Time of Crisis," cites several examples of effective community partnerships that the Department of Pediatrics utilized in Monroe County to provide continued pediatric care, behavioral health services, and food/meal distribution during the pandemic. The paper's co-authors argue that these community partnerships are critical for counteracting the damaging effects that the pandemic has on children and families from underrepresented communities, which include unemployment and reduced income for caregivers, school closures impacting daily schedules, and disruption of critical school wraparound services
"We felt that the emphasis on COVID impact was focused on economic outcomes with adults, so we wanted to give attention to the pediatric community and generate partnerships to address disparities," said lead author Jeff Yaeger, M.D. M.P.H., assistant professor from the Department of Public Health Sciences. Patrick Brophy, M.D. chair in the Department of Pediatrics, and Jeffrey Kaczorowski, M.D., professor in the Department of Pediatrics, were co-authors.
The study draws examples from past catastrophic events, such as the 1918 influenza pandemic, as well as Hurricanes Katrina and Sandy, to indicate that children and families living in poverty are at the highest risk of experiencing poor outcomes during crisis scenarios, including homelessness, unemployment, food insecurity, and trauma/violence.
Elaine Hill & Rena Patel Start Pregnancy Clinical Domain Team
Friday, October 9, 2020
The Pregnancy Clinical Domain Team co-led by Elaine Hill, PhD & Rena Patel, MD, MPH aims to leverage National COVID Cohort Collaborative data to gain insights into pressing COVID-19 questions around pregnancy. The goal is to understand incidence, timing, and severity in pregnant women, maternal and infant outcomes, and associated characteristics (clinical, demographic, environmental).
The team's first project has been approved to access data in the N3C Data Enclave: COVID-19 Incidence, Treatment, and Outcomes in Pregnant Women. This project seeks to understand associations between SARS-CoV-2 infection and treatment for COVID-19 with maternal and infant outcomes in the N3C cohort, and associations with maternal characteristics, including clinical and environmental factors, and COVID-19 severity among pregnant women. The project also aims to assess the likelihood of vertical transmission of SARS-CoV-2 from mother to infant and healthcare, and assess utilization during pregnant and postpartum periods among pregnant women.
Underrepresented populations suffer most from COVID-19 in nursing homes, assisted living communities
Tuesday, September 22, 2020
Older racial and ethnic minority residents in nursing homes and assisted living communities in the United States and their caregivers have been hit hardest by the Covid-19 pandemic, according to two new Medical Center research studies. The findings from the study led by Yue Li, a professor of public health sciences, are the first to document the disproportionate impact on residents from underrepresented racial and ethnic backgrounds in nursing homes across all states. Disparities of this magnitude, Li says, suggest that long-standing, fundamental inequalities in nursing homes resulting from segregated facilities with limited resources and poorest quality of care are being "exacerbated by the pandemic."
The second study, led by Helena Temkin-Greener, also a professor of public health sciences, was a first-ever empirical study involving the incidence of COVID-19 in US assisted living communities. "Immediate actions are needed to ensure that as the pandemic continues to evolve, nursing home residents from underrepresented racial/ethnic backgrounds, and the frontline workers caring for them, do not bear an additional later or sufferings due to systemic inequalities," reported the study's researchers.
The research was also featured on CNN.
Read Yue and Helena's new published studies:
Dr. Green Speaks at UR Alumni Event on Community Engagement
Monday, September 21, 2020
CCHP Community Health Policy & Education Director Dr. Theresa Green recently spoke at a UR alumni online learning event, titled "Community Engagement: Making the World Ever Better." In January 2020, for the first time, the University received the Carnegie Foundation's selective classification in community engagement. Dr. Green co-led the successful UR application for this classification. The alumni event explored the University's history of community engagement which led to this recognition, its current work with the community and commemorated Global Day of Service. In case you missed it, the event was taped and will soon be archived here.
Congratulations to Dr. Green!
Theresa Green elected as President of the Monroe County Board of Health
Thursday, September 17, 2020
Theresa Green, Assistant Professor of Public Health Sciences and the Director of Community Health Policy and Education at the Center for Community Health within the University of Rochester Medical Center, has been elected as President of the Monroe County Board of Health.
Congratulations!
Twylla Dillion Appointed Executive Director of HealthConnect One
Friday, September 11, 2020
Twylla Dillion, PhD graduate of our Health Services Research program has been appointed as the Executive Director of HealthConnect One. Since 1986, HealthConnect One (based in Chicago) has been the national leader in advancing respectful, community-based, peer-to-peer support for pregnancy, birth, breastfeeding and early parenting. Their vision is to see every baby, mother, and family thrive in a healthy community. We work to achieve this vision through an equity focused approach supporting the first 1000 days for birthing families.
Congratulations Twylla!
Xu, Intrator Publish Article in JAMDA
Friday, August 14, 2020
Former PhD Student, Huiwen Xu and current faculty member Orna Intrator have published a new paper in Journal of the American Medical Directors Association (JAMDA). Read Shortages of Staff in Nursing Homes During COVID-19 Pandemic: What Are the Driving Factors?
Paula Cupertino Awarded Grant From National Cancer Institute
Thursday, July 30, 2020
Congratulations to Paula Cupertino who has been awarded a grant (Administrative Supplement to Stimulate or Strengthen Global Cancer Health Disparities Research) for a clinical trial in Mexico by the Center for Global Health (National Cancer Institute). Congratulations!
Mitchell Wharton (Former MPH Grad student) authors paper about Health and Social Inequalities of HIV and COVID-19
Monday, July 13, 2020
Former MPH student and current Assistant professor of clinical nursing, Mitchell J. Wharton, PhD, RN, FNP-BC, CNS, has authored a paper, "Alarm at the Gate—Health and Social Inequalities are Comorbid Conditions of HIV and COVID-19."
COVID-19 Toll in Nursing Homes Linked to Staffing Levels and Quality
Thursday, June 18, 2020
A new study shows that residents of long-term care facilities with lower nurse staffing levels, poorer quality scores, and higher concentrations of disadvantaged residents suffer from higher rates of confirmed COVID-19 cases and deaths.
"In nursing homes, quality and staffing are important factors, and there already exists system-wide disparities in which facilities with lower resources and higher concentrations of socio-economically disadvantaged residents have poorer health outcomes," said Yue Li, Ph.D., a professor in the University of Rochester Medical Center (URMC) Department of Public Health Sciences and lead author of the study which appears in the Journal of the American Geriatrics Society. "These same institutional disparities are now playing out during the coronavirus pandemic."
Residents of long-term care facilities have been shown to be highly vulnerable to respiratory disease outbreaks, such as influenza or other common human coronaviruses. Current evidence suggests that COVID-19 disproportionately impacts older adults and individuals with chronic health conditions. These factors are more concentrated in nursing homes where residents are characterized by advanced age, more frequent and complex chronic disease patterns, and highly impaired physical, cognitive, and immune system functions, putting these populations at greater risk for more severe COVID-19 infections.
This phenomenon first came to light in a skilled nursing facility in the Seattle area in February during the early stages of the pandemic, where more than half of the residents in the facility became infected and a third died. Since that time, 50,000 coronavirus-related deaths, approximately 40 percent of the total, have been linked to nursing homes across the U.S.
The new study examined nursing home level data published on the Connecticut Department of Health and Human Services website. At the time of the study, Connecticut was one of the few states that made this information publically available. This information was compared to data from the Center for Medicare & Medicaid Service's (CMS) Nursing Home Compare website, which tracks quality, staffing, and health outcomes for nursing homes nationwide.
Analyses of the data showed that long-term care facilities with higher concentrations of disadvantaged residents, including Medicaid residents and racial and ethnic minorities, lower nurse staffing levels, particularly registered nurses (RN), and lower scores on CMS five-star quality measures, had higher rates of confirmed COVID-19 cases and deaths. Higher nurse staffing ratios in particular was strongly associated with fewer cases and deaths.
"In most nursing homes, RNs are the linchpin for the assessment and provision of medical care, including early identification of and response to emergencies and life threatening situations," said Li. "Our findings of the strong negative association between RN staffing and the number of COVID-19 cases and deaths in nursing homes are consistent with research that has demonstrated that increased nursing levels are key to an institution's ability to respond to outbreaks of emerging infections."
New Paper Published by Alio on Self-Reported Experiences of Racial Discrimination Among African Americans in Upstate New York
Wednesday, June 17, 2020
Associate Professor, Amina Alio, PhD has published a new paper in the Journal of Black Studies about Self-Reported Experiences of Racial Discrimination Among African Americans in Upstate New York. Dr. Alio has extensive experience in community-based participatory research, qualitative and quantitative methods, and evaluation design. Her research areas include racial/ethnic health disparities and global health. Specifically, Dr. Alio focuses on the impact of behavioral, psychosocial and environmental factors on pregnancy outcomes, particularly among African Americans. Her international research is in women's reproductive health, HIV prevention, intimate partner violence and pregnancy outcomes in sub-Saharan Africa.
Fatal Opioid Overdoses May Be More Common Than Thought
Tuesday, May 19, 2020
Opioids have been blamed for the deaths of at least 400,000 U.S. residents in the past two decades—but research now shows that number could be much higher.
Researchers looked at data from the Centers for Disease Control and Prevention on about 630,000 people who died of drug overdoses between 1999 and 2016. They separated the deaths into two categories: those with and without a specific drug indicated.
For the first category, they analyzed how contributing causes of death (such as injuries and heart problems) and personal characteristics (such as age and gender) correlated with opioid involvement. They then used these analyses to calculate the probability of opioid involvement for each unidentified drug overdose, and they found that the number of opioid deaths is likely 28 percent higher than generally reported.
Theodore Brown receives Lifetime Achievement Award from American Association for the History of Medicine
Wednesday, May 13, 2020
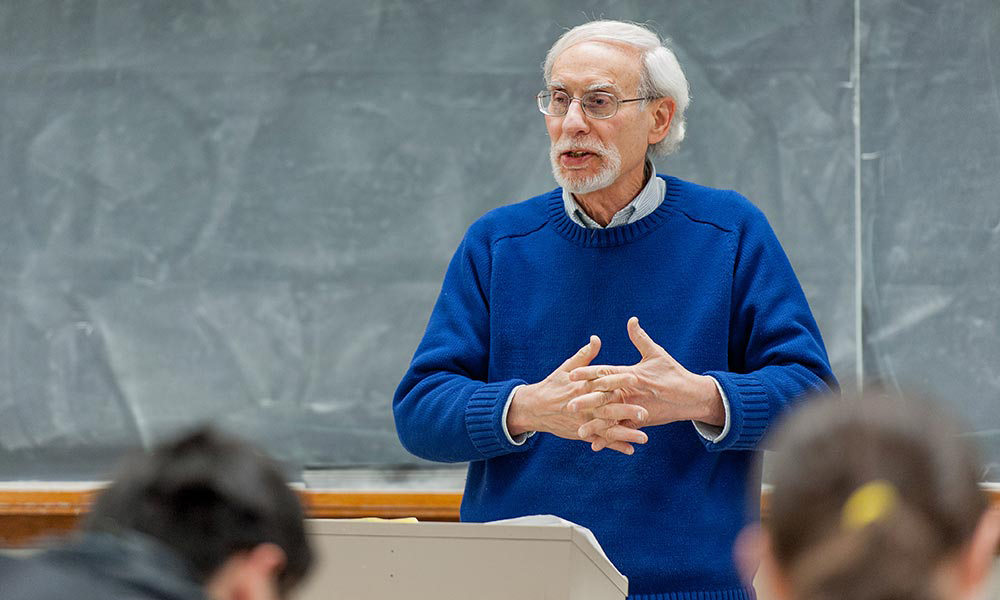
Over the course of his distinguished career, Theodore Brown, professor emeritus of history and public health sciences has “advanced the cutting edge of medical historical scholarship and shaped the work of other historians.” (University of Rochester photo / Brandon Vick)
Theodore Brown, a University of Rochester professor emeritus of history and public health sciences, is the recipient of this year's Genevieve Miller Lifetime Achievement Award from the American Association for the History of Medicine (AAHM).
Over the course of a long and distinguished career, Brown has been "a major contributor to the historical understanding of US health policy and politics, as well as the history of both US and international public health," says John Harley Warner, the Avalon Professor of the History of Medicine at Yale University and a member of the AAHM's Lifetime Achievement Award committee.
First established in 1988, the lifetime award is given annually to a member of the association who has retired from regular institutional practice with a distinguished record of support for the history of medicine, and who has continued to make important scholarly contributions.
Brown's research interests run the gamut from US health policy and politics, to the history of psychosomatic medicine, stress research, and biopsychosocial approaches to clinical practice. Prior to his retirement in 2018, he had been the University's inaugural Charles E. and Dale L. Phelps Professor of Public Health and Policy, a position he held for five years.
His articles and coauthored books, among them Making Medical History: The Life and Times of Henry E. Sigerist (Johns Hopkins University Press, 1997), Comrades in Health: US Health Internationalists, Abroad and at Home (Rutgers University Press, 2013), and a comprehensive history of the World Health Organization published in 2019 by Cambridge University Press— along with his "critical labor" in editing the Rochester Studies in the History of Medicine book series and a regular historical section for the American Journal of Public Health—"have advanced the cutting edge of medical historical scholarship and shaped the work of other historians," says Warner. "Through his scholarship, mentorship, and leadership in organizations such as the Sigerist Circle of the American Association for the History of Medicine, he has been particularly instrumental in infusing issues of health activism, health disparities, and the American health left into the fabric of the mainstream history of medicine and public health."
Gloria Culver, dean of the University's School of Arts & Sciences, hails Brown for his leadership and collegiality. "He is a wonderful scholar and his impact on the field will be felt for years to come. My first thoughts when I heard the news was that this is not surprising—it's so very well deserved. Ted is a leader and an amazing colleague."
Among the books Brown has authored or coauthored is the whimsical The Quest for Health Care Reform: A Satirical History, published by the American Public Health Association in 2012.
Chunkit Fung Receives Human Rights Leadership Award
Tuesday, May 12, 2020
Chunkit Fung, M.D., associate professor of Medicine and Public Health Sciences, received the Human Rights Campaign (HRC) Leadership Award from Rising Star Gala Leaders at the HRC Equality Convention held on May 1. Fung received his award in recognition of his dedication in leading the HRC Western New York Dinner Committee and for his fundraising efforts.
The HRC Western NY Chapter provides resources and hosts regular local events to support the LGBTQ community in Western NY, including HRC second Thursday network event and Annual Western NY HRC Dinner, a fundraiser that showcases and supports the work of the Human Rights Campaign.
The University of Rochester, including URMC, has been a sponsor for this event for the past three years. Strong Memorial, Highland and Thompson Hospitals have been designated by the HRC as national leaders in LGBTQ healthcare.
Social distancing has stabilized, but failed to reverse, the spread of COVID-19
Tuesday, May 12, 2020
As policymakers try to restart the economy but also control COVID-19, data scientists at Cornell University and the University of Rochester are studying the impacts of social distancing. While social distancing has effectively slowed the spread of COVID-19, the measures have not reduced the total number of daily new cases.
"The effect is not as large as one would have hoped for going in," says lead author Aaron Wagner, professor of electrical and computer engineering at Cornell University. As a result, he says, the states now reopening businesses and relaxing restrictions "do not have much headroom" for error. "You're right on the edge of it starting to blow up again."
"Policy makers need to be aware of this," says co-author Elaine Hill, assistant professor of public health sciences at the University of Rochester. "We need more studies to identify the practices that can move us to a place where COVID-19 is actually contracting."
The study authors suggest that policymakers:
- Consider a carefully phased relaxation of social distancing, such as first targeting a limited number of businesses and economic activities where duration of human contact is limited: restaurants offering take-out meals, for example, rather than in-restaurant dining; or construction activity where it might be easier to maintain social distancing between workers.
- Allow enough time for models like the one used in this study to assess the effect of the targeted relaxations before extending them to other areas.
- Consider augmenting social distancing with other practices, such as universal use of face masks, or contact tracing.
Epidemiology Alumnus AnnaLynn Williams Gives CPD/URBEST Career Story
Saturday, May 2, 2020
CPD/URBEST Career Story w/ AnnaLynn Williams, Ph.D.- What to think about when applying for NIH Fellowship and Transition Awards and planning for the pre- to post-doc transition.
May 1 recorded session available at this link.
#ThankYouPublicHealth! from NPHW.org
Friday, April 17, 2020
Timmy Li, URMC Epidemiology PhD Graduate in NY Post as "Hero of the Day"
Monday, April 13, 2020
Volunteer EMT Timmy Li normally spends his free time treating injured runners and cyclists in Central Park.
But as the Big Apple gets crushed with 911 calls due to the coronavirus pandemic, he's now devoting his nights and weekends to far more serious emergencies, far outside the park's borders.
"When it was declared a pandemic, I told myself, 'as long I am not sick myself and as long as I'm available, I will continue to take shifts and calls,'" Li, 30, told The Post.
"Pretty much every 911 call right now is COVID related. Almost everything. We still have the injuries, the car crashes, but almost everything is a potential COVID call."
The Queens resident, who also works full-time as a clinical researcher at Northwell Health, is part of the Central Park Medical Unit, a team of 150 volunteer EMTs who typically patrol the park's 843 acres.
But as emergency calls skyrocket past previous records and hordes of EMTs call out sick, the team has now stepped up to handle emergency calls across Manhattan under the FDNY's Mutual Aid system.
"We're working almost 24/7," Li said. "It's definitely challenging, physically exhausting, and mentally exhausting knowing that a lot of people are dying."
The medic, who holds a doctorate in epidemiology, said his unit is used to disaster response, but the coronavirus is a whole different monster.
"We have responded to things like 9/11, Hurricane Sandy, the blackout and the heat wave last summer. And those feel a little different in that those, the risk of me getting infected or injured was low. But this is very real," Li said.
Today starts the 25th National Public Health Week!
Monday, April 6, 2020
#PublicHealth provides critical services & infrastructure, its work & impacts are often invisible, taken for granted.... except in a crisis ..... Today starts the 25th National Public Health Week. Kudos to the PH workforce everyday!#NPHW
-Ann Dozier, RN, PhD, FAAN
Professor and Chair, Public Health Sciences
Robert Block Named to Northeast Lipid Association Board
Tuesday, March 31, 2020
Robert Block, M.D., M.P.H., FACP, FNLA, professor of Public Health Sciences, Medicine and in the Center for Community Health and Prevention, was recently named to serve a three-year term on the Northeast Lipid Association Board of Directors (the regional chapter of the National Lipid Association) beginning in June.
Block specializes in the care of patients with complex lipid disorders including familial cholesterol disorders and directs the URMC Lipid Apheresis Program.
LETTER: Coronavirus and vaping — pandemic meets epidemic
Wednesday, March 25, 2020
To the Editor:
The World Health Organization has declared COVID-19 to be a pandemic. The U.S. Surgeon General declared teen vaping a national epidemic. Research will show how much they are linked, but evidence already supports advice to quit vaping (and smoking) to help protect people from COVID-19.
Both vaping and smoking damage the lungs, and the recent vaping-related outbreak of lung disorders shows how serious that damage can be. People with weaker lungs are less able to fend off the effects of coronavirus, and people who have lung disease are at higher risk of more serious coronavirus illness.
In all the messaging about hand-washing and social distancing to prevent coronavirus, we also need to emphasize the importance of quitting smoking and vaping.
To stop vaping or smoking, contact your doctor and the NYS Smokers' Quitline at 1 (866) 697-8487 and at nysmokefree.com.
SCOTT McINTOSH, PhD
Public Health Sciences, University of Rochester
Twenty Presentations Scheduled for HSR Faculty and Students at Top Academic Conferences in June 2020
Wednesday, March 25, 2020
Twenty presentations are scheduled for HSR faculty and students at two national academic conferences in health services research, AcademyHealth and ASHEcon (American Society of Health Economists) this year. Among them, twelve are scheduled as podium presentations.
AcademyHealth and ASHEcon attract scholars from worldwide to present the results of their pioneering research. Presentations for both meetings are selected on a highly competitive base.
HSR Abstracts Accepted by 2020 Annual Meeting of Academy Health & ASHEcon
|
Authors List |
Title |
Topic Section |
Time of Presentation |
Format |
Conference |
|
Helena Temkin-Greener, Yunjiao Mao, Susan Ladwig, Brian McGarry, Yue Li |
State Variations in Regulatory Stringency for Assisted Living Communities: Potential Implications for Service Supply, Cost, and Quality |
Understanding the Variation in Home and Community Based Care |
06/14/2020, 2:15PM |
Podium |
AcademyHealth |
|
Yue Li, Xueya Cai, Shan Gao, Yeates Conwell, Adam Simning, Helena Temkin-Greener |
Attempted Suicide and Self-Inflicted Injury Among US Nursing Home Residents: Resident and Facility Correlates |
Caring for High Risk Nursing Home Patients |
06/15/2020, 11:30AM |
Podium |
AcademyHealth |
|
Sijiu Wang, Helena Temkin-Greener, Adam Simning, R. Tamara Konetzka, Shubing Cai |
Is the Generosity of Medicaid Home and Community-Based Services Associated with Community Discharge from Skilled Nursing Facilities? |
Understanding the Variation in Home and Community Based Care |
06/14/2020, 2:15PM |
Podium |
AcademyHealth |
|
Sijiu Wang, Di Yan, Helena Temkin-Greener, Shubing Cai |
Does Medicaid HCBS Generosity Influence Nursing Home Placement for Dually Eligible ADRD Patients? |
Understanding the Variation in Home and Community Based Care |
06/14/2020, 2:15PM |
Podium |
AcademyHealth |
|
Jessica Orth, Yue Li, Adam Simning, Sheryl Zimmerman, Helena Temkin-Greener |
Nursing Home Residents with Dementia Experience Better End-of-Life Care and Outcomes in Nursing Homes with Alzheimer's Special Care Units? |
Quality Outcomes at the End-of-Life: Incorporating Patient Preferences and Values |
06/14/2020, 4:15PM |
Podium |
AcademyHealth |
|
Alina Denham, Peter Veazie |
An explanatory model of care seeking: Understanding how factors drive motivation |
What Does All This Data Mean? Conceptual Frameworks, Theoretical Explanations, Mechanisms, and Models |
06/15/2020, 3:00PM |
Podium |
AcademyHealth |
|
Meiling Ying, Caroline Thirukumaran, Xueya Cai, Yue Li |
Mandatory Medicare Bundled Payment Program for Lower Extremity Joint Replacement Is Associated with More Efficient Post-Acute Care but Maintained Disparities between Medicare-Only and Dual Eligible Patients |
Impact of Medicare Payment Models on Spending and Quality of Care |
06/14/2020, 8:45AM |
Podium |
AcademyHealth |
|
Di Yan, Sijiu Wang, Helena Temkin-Greener, Shubing Cai |
Hcbs Service Intensity and Nursing Home Placement for Patients with Alzheimer's Disease and Related Dementias: Does Race Matter? |
Social Determinants of Health and Their Influence on Health and Health Care among Older Adults and People with Disabilities |
06/15/2020, 9:45AM |
Podium |
AcademyHealth |
|
Tianwen Huan, Orna Intrator |
Provision of VA Long Term Services and Supports (LTSS) and Inpatient Care to Veterans Residing in Deprived Areas |
Incorporating Social Services to Improve Outcomes for Complex Patients |
06/15/2020, 11:30AM |
Podium |
AcademyHealth |
|
Alina Denham, Elaine Hill, David Slusky, Janet Currie |
Evaluation of Initiatives to Improve Maternal Health in New York State |
Effects of Public Policy on Maternal Health |
06/08/2020,10:15AM |
Podium |
ASHEcon |
|
Alina Denham, Andrew Boslett, Tarsha Vasu, Michael Mendoza, Elaine Hill |
Medical Examiner Vs Coroner: Does It Matter for the Opioid Epidemic? |
Investigations into the Opioid Epidemic? |
06/10/2020, 8:30AM |
Podium |
ASHEcon |
|
Yeunkyung Kim, Caroline Thirukumaran, Helena Temkin-Greener, Elaine Hill, Robert Holloway, Yue Li |
The Effect of Medicare Shared Savings Program on Readmissions and Variations by Race and Payer Status |
Moving to Value in the Medicare Program |
06/10/2020, 10:15AM |
Podium |
ASHEcon |
|
Shubing Cai, Sijiu Wang, Helena Temkin-Greener |
Obesity, Dementia and Antipsychotic Use Among Nursing Home Residents |
Poster Session: Aging, Disability, and End-of-Life |
06/15/2020, 8:00AM |
Poster |
AcademyHealth |
|
Caroline Thirukumaran, Xueya Cai, Laurent Glance, Yeunkyung Kim, Benjamin Ricciardi, Kevin Fiscella, Yue Li |
Geographic variation and disparities in use of hip and knee replacement: 2009 to 2017 |
Poster Session: Disparities and Health Equity |
06/15/2020, 8:00AM |
Poster |
AcademyHealth |
|
Yunna Xie, Peter Veazie, Inkyu Kim, Alice Pentland, Brian Pentland and Julie Wolf |
Visit Complexity: A Novel Quality Measure of Healthcare Resources Allocation in Disparity Study |
Poster Session: Measuring Safety, Quality, and Value |
06/14/2020, 12:30PM |
Poster |
AcademyHealth |
|
Jessica Orth, Yue Li, Adam Simning, Helena Temkin-Greener |
Aggressive Behaviors, Suicidal Ideation, and Depression in US Nursing Homes: Association with the Availability of Behavioral Health Services? |
Poster Session: Aging, Disability, and End-of-Life |
06/15/2020, 8:00AM |
Poster |
AcademyHealth |
|
Huiying Wang, Wei Song, Bruce Kinosian, Edward Miller, Orna Intrator |
Characteristics of Long-stay Veterans in VA Community Living Centers, State Veterans Homes and Community Nursing Homes |
Poster Session: Aging, Disability, and End-of-Life |
06/15/2020, 8:00AM |
Poster |
AcademyHealth |
|
Di Yan, Sijiu Wang, Helena Temkin-Greener, Shubing Cai |
Home and Community-Based Services Use by Medicare-Medicaid Dually Eligible Users with Alzheimer's Disease and Related Dementias: Racial Differences in Service Use and Outcomes |
Poster Session: Aging, Disability, and End-of-Life |
06/15/2020, 8:00AM |
Poster |
AcademyHealth |
|
Wenhan Guo, Yue Li, Helena Temkin-Greener |
The Association between Nursing Home Patient Safety Culture and Discharge Outcomes for Post-Acute Care Residents |
Poster Session: Aging, Disability, and End-of-Life |
06/15/2020, 8:00AM |
Poster |
AcademyHealth |
|
Alina Denham, Elaine Hill, Maria Raven, Michael Mendoza, Peter Veazie |
Are Emergency Department and Primary Care Substitutes or Complements in Medicaid: An Explanation of an Unintended Effect of the ACA Medicaid Expansions |
Poster Session |
06/09/2020,5:15PM |
Poster |
ASHEcon |
The death toll of the opioid epidemic is higher than originally thought, researchers say
Friday, February 28, 2020
Opioid-related overdoses could be 28 percent higher than reported because of incomplete death records, researchers found in a study published Thursday.
More than 400,000 people in the United States have died of opioid overdoses since the turn of the century, a quarter of them in just the past six years. But University of Rochester researchers found that between 1999 and 2016, about 100,000 more people died from opioids who were not accounted for — potentially obscuring the scope of the opioid epidemic and affecting funding for government programs intended to confront it, Elaine Hill, an economist and senior author of the study, told The Washington Post.
The discrepancies were most pronounced in several states, including Alabama, Mississippi, Pennsylvania, Louisiana and Indiana.
"We thought we would find underreporting, but we were definitely not prepared to find how spatially determined it is," Hill said.
University Earns First Community Engagement Classification from Carnegie Foundation
Monday, February 3, 2020
The University has received 2020 Carnegie Community Engagement Classification, an elective designation that indicates institutional commitment to community engagement. This is the first time that the University has earned the classification from the Carnegie Foundation for the Advancement of Teaching, becoming one of 359 institutions nationwide to hold the distinction.
Vaping Linked to Higher Risk of Self-Reported COPD Diagnosis
Thursday, January 2, 2020
A new study reveals an elevated risk of self-reported chronic obstructive pulmonary disease (COPD) — the third leading cause of death associated with smoking — among people using e-cigarettes. People who vaped were at increased risk even if they had never smoked tobacco, which casts doubt on e-cigarette companies' claims that vaping is a safe alternative to smoking.
According to the study, people who vaped were at a 47-percent greater risk of self-reported COPD diagnosis as compared to people in the study who did not use tobacco products. Compared to ex-smokers, people who had quit smoking and switched to e-cigarettes were 27 percent more likely to report a COPD diagnosis.
The study, published by Nicotine and Tobacco Research, is based on 2016 and 2017 Behavioral Risk Factor Surveillance System (BRFSS) national survey data of nearly one million adults. Survey participants were asked whether they had ever been diagnosed with COPD by their health-care provider.
Authors of the study, which was funded in part by the University of Rochester Clinical and Translational Science Institute (UR CTSI), the National Cancer Institute and the Food and Drug Administration, are Zidian Xie, Ph.D., Deborah J Ossip, Ph.D., Irfan Rahman, Ph.D. and Dongmei Li, Ph.D.
"It is clear, based on the large sample size of this study, that there is a significant link between vaping and self-reported COPD diagnosis in adults, even among vapers who never smoked before," said lead study author Zidian Xie.
Senior study author Dongmei Li, an associate professor in the UR CTSI, added, "More long-term clinical research is needed to determine how e-cigarette use is related to COPD, but our findings are consistent with other recent studies showing that e-cigarette use is associated with respiratory issues."
"This study provides further evidence that vaping simply isn't safe," said Deborah Ossip, a tobacco research expert and professor of Public Health Sciences at the University of Rochester Medical Center. "We hope that people begin to heed this message, especially young people who think vaping is cool and who are enticed by the thousands of available flavors."
Recent statistics from the Center for Diseases Control and Prevention's National Youth Tobacco Survey demonstrated the popularity of vaping among young people in the U.S. About one of every 10 middle school students and one out of four high school students reported in 2019 that they used electronic cigarettes.