News
Cassandra Houser Receives AAI Young Investigator Award at the 22nd Annual Upstate New York Immunology Conference
Wednesday, November 6, 2019
IMV Ph.D. Graduate Student, Cassandra Houser (Paige Lawrence's Lab) received one of ten AAI Young Investigator Awards at the 22nd Annual Upstate New York Immunology Conference. The conference this year took place October 28th at Albany Medical Center. The award is based on the top poster abstracts submitted based on scientific rigor and significance to the field of immunology.
Congrats Cassandra!
University of Rochester Researchers Discuss Vaping-Related Lung Injury on the Today Show
Thursday, October 31, 2019
University of Rochester Environmental Health Sciences Center members Daniel Croft, M.D., M.P.H., and Irfan Rahman, Ph.D., were featured on a Today Show segment about vaping-related lung injury. In the segment, Rahman is shown working in his lab while Croft discussed the symptoms associated with this condition.
Rahman uses cell, mouse, and human studies to investigate how flavoring chemicals used in vaping devices affect lung health. He also analyzes vaping liquid collected from patients and hospitals around the world to better understand its chemical makeup. Croft, a clinician researcher who focuses on inhalation toxicology, helps interpret the clinical relevance of findings from the lab and collaborates on a study to better understand respiratory effects in people who vape.
Medical Student Gordon Wong presents at the annual URMC Medical School poster session
Monday, October 21, 2019
Dr. Georas (left) and Gordon Wong
Medical Student Gordon Wong presented a poster at the annual URMC Medical School poster session, describing his summer research project. Gordon studied how protein kinase D regulates airway inflammation and epithelial barrier integrity in mouse models of airway inflammation and viral infections. He made some very exciting discoveries, working with graduate student Janelle Veazey, specifically elucidating how protein kinase D controls the recruitment of neutrophils to the lungs.
How environmental toxins impair immune system over multiple generations
Thursday, October 17, 2019
New research shows that maternal exposure to a common and ubiquitous form of industrial pollution can harm the immune system of offspring and that this injury is passed along to subsequent generations, weakening the body's defenses against infections such as the influenza virus.
The study was led by Paige Lawrence, Ph.D., with the University of Rochester Medical Center's (URMC) Department of Environmental Medicine and appears in the Cell Press journal iScience. The research was conducted in mice, whose immune system function is similar to humans.
"The old adage 'you are what you eat' is a touchstone for many aspects of human health," said Lawrence. "But in terms of the body's ability to fights off infections, this study suggests that, to a certain extent, you may also be what your great-grandmother ate."
While other studies have shown that environmental exposure to pollutants can have effects on the reproductive, respiratory, and nervous system function across multiple generations, the new research shows for the first time that the immune system is impacted as well.
This multigenerational weakening of the immune system could help explain variations that are observed during seasonal and pandemic flu episodes. Annual flu vaccines provide some people more protection than others, and during pandemic flu outbreaks some people get severely ill, while others are able to fight off the infection. While age, virus mutations, and other factors can explain some of this variation, they do not fully account for the diversity of responses to flu infection found in the general population.
"When you are infected or receive a flu vaccine, the immune system ramps up the production of specific kinds of white blood cells in response," said Lawrence. "The larger the response, the larger the army of white blood cells, enhancing the ability of the body to successfully fight off an infection. Having a smaller size army — which we see across multiple generations of mice in this study — means that you're at risk for not fighting the infection as effectively."
In the study, researchers exposed pregnant mice to environmentally relevant levels of a chemical called dioxin, which, like polychlorinated biphenyls (PCBs), is a common by-product of industrial production and waste incineration, and is also found in some consumer products. These chemicals find their way into the food system where they are eventually consumed by humans. Dioxins and PCBs bio-accumulate as they move up the food chain and are found in greater concentrations in animal-based food products. The scientists observed the production and function of cytotoxic T cells — white blood cells that defend the body against foreign pathogens, such as viruses and bacteria, and seek out and destroy cells with mutations that could lead to cancer — was impaired when the mice were infected with influenza A virus.
Rochester Researchers Receive $12 Million Award to Visualize the Immune System in Action
Wednesday, October 16, 2019
NIH grant will help identify new strategies to enhance immune response
 Cutting-edge imaging technologies that allow scientists to watch the immune system work in real time are leading to a greater understanding of how we combat infection and disease. With a new $12 million grant, researchers will use this knowledge to explore strategies to better fight infections like the flu and beat back overactive immune responses in disorders like rheumatoid arthritis and lupus.
Cutting-edge imaging technologies that allow scientists to watch the immune system work in real time are leading to a greater understanding of how we combat infection and disease. With a new $12 million grant, researchers will use this knowledge to explore strategies to better fight infections like the flu and beat back overactive immune responses in disorders like rheumatoid arthritis and lupus.
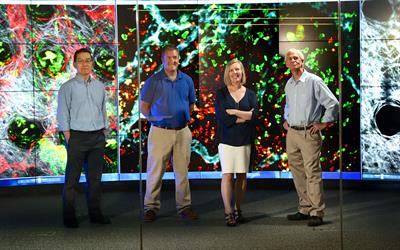
The five-year project, led by Deborah J. Fowell, Ph.D., Dean's Professor in the department of Microbiology and Immunology at the University of Rochester Medical Center, builds on a $9 million grant that her team received in 2014. Both program project grants were awarded by the National Institute of Allergy and Infectious Diseases at the National Institutes of Health.
"When we take cells out of their natural environment and study them in a dish we're missing out on a lot of biology," said David J. Topham, Ph.D., a study project leader and professor of Microbiology and Immunology at URMC. "Imaging and tracking live cells is an emerging theme in immunology and one that I think is going to move forward meaningful discoveries in the field."
In addition to Fowell and Topham, project leaders include Minsoo Kim, Ph.D.,James F. Miller, Ph.D., and Patrick Oakes, Ph.D. Scientists from Cornell and Loyola University will collaborate with the team, as well.
Environmental Toxins Impair Immune System over Multiple Generations
Wednesday, October 2, 2019
New research shows that maternal exposure to a common and ubiquitous form of industrial pollution can harm the immune system of offspring and that this injury is passed along to subsequent generations, weakening the body's defenses against infections such as the influenza virus.
The study was led by Paige Lawrence, Ph.D., with the University of Rochester Medical Center's (URMC) Department of Environmental Medicine and appears in the Cell Press journal iScience. The research was conducted in mice, whose immune system function is similar to humans.
"The old adage 'you are what you eat' is a touchstone for many aspects of human health," said Lawrence. "But in terms of the body's ability to fights off infections, this study suggests that, to a certain extent, you may also be what your great-grandmother ate."
While other studies have shown that environmental exposure to pollutants can have effects on the reproductive, respiratory, and nervous system function across multiple generations, the new research shows for the first time that the immune system is impacted as well.
This multigenerational weakening of the immune system could help explain variations that are observed during seasonal and pandemic flu episodes. Annual flu vaccines provide some people more protection than others, and during pandemic flu outbreaks some people get severely ill, while others are able to fight off the infection. While age, virus mutations, and other factors can explain some of this variation, they do not fully account for the diversity of responses to flu infection found in the general population.
"When you are infected or receive a flu vaccine, the immune system ramps up production of specific kinds of white blood cells in response," said Lawrence. "The larger the response, the larger the army of white blood cells, enhancing the ability of the body to successfully fight off an infection. Having a smaller size army -- which we see across multiple generations of mice in this study -- means that you're at risk for not fighting the infection as effectively."
In the study, researchers exposed pregnant mice to environmentally relevant levels of a chemical called dioxin, which, like polychlorinated biphenyls (PCBs), is a common by-product of industrial production and waste incineration, and is also found in some consumer products. These chemicals find their way into the food system where they are eventually consumed by humans. Dioxins and PCBs bio-accumulate as they move up the food chain and are found in greater concentrations in animal-based food products.
URMC scientist leading nation with vaping research on effects of flavored e-liquids
Thursday, September 26, 2019
New York Gov. Andrew Cuomo is looking to expand the state's newly implemented ban on flavored e-cigarettes to include menthol.
On Thursday, the Democratic governor directed the state's health commissioner to convene an emergency meeting as soon as possible to take steps to include menthol in the first-in-the-nation ban to ban the sale of flavored e-cigarettes. The ban currently excludes tobacco and menthol flavors.
The announcement comes as one local researcher is leading the nation in studying the effects of flavored e-liquids.
Dr. Irfan Rahman with URMC has been researching e-cigarettes in his lab at the School of Medicine for the better part of a decade. The lab has allowed the scientist to take a closer look at vaping and its effects on the body. A few years ago, Dr. Rahman started looking at the makeup of the flavors.