News
Understanding gene therapy for babies and young children
Tuesday, October 29, 2024

When a parent hears their newborn or young child has a genetic condition that could affect the rest of their lives, they may be scared, confused, and have questions about what to do next. Research in gene therapy has led to significant changes in how doctors work with families on those questions.
This hour, we sit down with two local mothers who share their families’ stories of accessing care for their children, and we’re joined by the experts who provide that care.
Our guests:
- Emily Hessney Lynch, parent of a child who received gene therapy
- Kate White, DPT, physical therapist in the Orthopedics Department at the University of Rochester Medical Center, and creator of Team Teddy 5K, an annual fundraiser for Duchenne Muscular Dystrophy research
- Samuel Mackenzie, M.D., Ph.D., assistant professor in the Departments of Neurology, Neuroscience, and Pediatrics; and the Center for Health and Technology at the University of Rochester Medical Center
- Bo Hoon Lee, M.D., assistant professor in the Departments of Pediatrics and Neurology, Child Neurology at the University of Rochester Medical Center
Comparing gene sequences across species to understand aging and dementia
Wednesday, October 16, 2024
A new grant partners longevity researchers and Alzheimer’s experts at Rochester to study the gene mechanisms that contribute to long and healthy lifespans
Whether you give a mouse a cookie, as the book title goes, or kale leaves, or hot-stone massages, they will not live longer than two to three years. But other mammals, like naked mole rats and bowhead whales, can live much longer—and perhaps can teach us to follow suit.
At the University of Rochester, a new collaboration between leading longevity researchers and brain disease experts examines gene mechanisms responsible for long life, drawing on the latest findings to pursue novel interventions for the treatment and prevention of Alzheimer’s disease and related dementias.
Today’s oldest naked mole rats, born during the Reagan administration, show exceptional resistance to age-related disease. Meanwhile, when degus (small Chilean rodents) develop Alzheimer’s disease, it progresses in a remarkably similar manner to humans. Examining the genes of these mammals has the potential to yield insights into how humans can live longer—with their cognitive faculties intact.
“No matter how much you pamper a mouse, it will not live to 40 years as naked mole rats will,” says Vera Gorbunova, the Doris Johns Cherry Professor in the departments of biology and of medicine. To bridge the knowledge gap from rodents, whales, and other long-lived mammals to humans, Gorbunova tapped M. Kerry O’Banion, a professor of neuroscience at the University of Rochester Medical Center, who has studied the pathogenesis of Alzheimer’s disease for 30 years.
Read More: Comparing gene sequences across species to understand aging and dementiaFDA Taps URMC to Develop New Digital Measures for Huntington's Disease
Wednesday, October 9, 2024
New funding will enable researchers to determine whether subtle early signs of Huntington's disease can be detected by wearable sensors. Developing digital tools to identify objective measures of this complex disease will help accelerate the development of new therapies. The study will be led by the University of Rochester’s Center for Health + Technology, which has been studying digital health technologies in Parkinson's disease for a decade.
“Similar to Parkinson's, our traditional measures of Huntington's disease are subjective, episodic, and have not reliably been sensitive to progression, especially in early disease,” said University of Rochester Medical Center (URMC) neurologist Jamie Adams, MD, principal investigator of the new study. "Huntington's is a genetic disease with a long pre-symptomatic stage. This study employs a new staging system and focuses on the early stages, which are the likely target populations of disease-modifying clinical trials."
The new research is being funded by the Food and Drug Administration (FDA), under the Digital Health Technologies for Drug Development program. The FDA has tasked URMC and collaborators with demonstrating the reliability, validity, and meaningfulness of two key digital measures: daily living mobility (gait) and chorea, the involuntary muscle movements that are a hallmark symptom of the disease. Data will be captured remotely and continuously using wrist and trunk-worn digital sensors in individuals with early-stage Huntington's disease and controls. The study also includes qualitative work using an innovative symptom mapping approach to ensure meaningfulness of the measures to people with Huntington’s disease.
Read More: FDA Taps URMC to Develop New Digital Measures for Huntington's DiseaseCelebrating Decades of Advances in Myotonic Dystrophy Research
Tuesday, September 17, 2024
 On September 15, Strong Memorial Hospital lit up blue to commemorate Myotonic Dystrophy Awareness Day and the significant scientific progress achieved in Rochester and beyond over the past 30 years. These advancements have brought researchers closer than ever to developing treatments for this debilitating disease.
On September 15, Strong Memorial Hospital lit up blue to commemorate Myotonic Dystrophy Awareness Day and the significant scientific progress achieved in Rochester and beyond over the past 30 years. These advancements have brought researchers closer than ever to developing treatments for this debilitating disease.
The recent renewal of a joint University of Rochester Medical Center (URMC) and University of Florida Paul D. Wellstone Muscular Dystrophy Cooperative Research Center will further strengthen these efforts. URMC, one of the original Wellstone Centers established in 2003, has been continuously funded by the National Institutes of Health to study myotonic dystrophy and facioscapulohumeral muscular dystrophy.
"The Wellstone Center program has been instrumental in our understanding of the molecular and physiological processes underlying the most common form of adult-onset muscular dystrophy, myotonic dystrophy," said Charles Thornton, MD, co-director of the Wellstone Center. "This knowledge has enabled us to develop promising treatments for this disease. The center's organization, which includes the National Registry for myotonic dystrophy, is built upon strong and longstanding collaborations between basic researchers at the University of Florida and clinical experts at the University of Rochester."
The new funding will support research in Rochester and Florida aimed at accelerating clinical research for novel gene therapies in myotonic dystrophy, type one (DM1), and prepare to translate these therapies into clinical practice, if approved. It is anticipated that modified versions of these therapies could also be effective for myotonic dystrophy, type two (DM2). To expedite clinical trials for DM2, researchers will expand their basic and clinical research efforts in this area.
Researchers at the University of Rochester Medical Center have been at the forefront of these advancements. Over three decades ago, Robert (Berch) Griggs, MD, Richard Moxley, MD, and Thornton were the first to describe myotonic dystrophy type 2. In collaboration with patients and families, the national registry has been an invaluable resource for understanding the natural history of the disease and conducting clinical research.
Read More: Celebrating Decades of Advances in Myotonic Dystrophy ResearchCleaning up the aging brain
Thursday, August 15, 2024
Rochester scientists are restoring the brain’s trash disposal system with a drug currently used to induce labor
Alzheimer’s, Parkinson’s, and other neurological disorders can be seen as “dirty brain” diseases, where the brain struggles to clear out harmful waste. Aging is a key risk factor because, as we grow older, our brain’s ability to remove toxic buildup slows down. However, new research in mice demonstrates that it’s possible to reverse age-related effects and restore the brain’s waste-clearing process.
“This research shows that restoring cervical lymph vessel function can substantially rescue the slower removal of waste from the brain associated with age,” says Douglas Kelley, a professor of mechanical engineering at the University of Rochester. “Moreover, this was accomplished with a drug already being used clinically, offering a potential treatment strategy.”
Kelley is one of the lead authors of the study, which appears in the journal Nature Aging, along with Maiken Nedergaard, codirector the University’s Center for Translational Neuromedicine. The study is one of many collaborations carried out by researchers at Rochester’s Hajim School of Engineering & Applied Sciences and the Medical Center.
First described by Nedergaard and her colleagues in 2012, the glymphatic system is the brain’s unique waste removal process that uses cerebrospinal fluid (CSF) to wash away excess proteins generated by energy-hungry neurons and other cells in the brain during normal activity. The discovery pointed the way to potential new approaches to treat diseases commonly associated with the accumulation of protein waste in the brain, such as Alzheimer’s (beta amyloid and tau) and Parkinson’s (alpha-synuclein). In healthy and young brains, the glymphatic system does a good job of flushing away these toxic proteins; however, as we age, this system slows, setting the stage for these diseases.
Read More: Cleaning up the aging brainURMC Named Batten Disease Center of Excellence
Tuesday, July 23, 2024

The Batten Disease Support and Research Association (BDSRA) Foundation has designated the University of Rochester Batten Center (URBC) as a Center of Excellence. This recognition highlights URBC’s dedication to providing specialized multidisciplinary care and advancing research for Batten diseases, a collection of rare and fatal neurodegenerative disorders affecting children.
This announcement, made at the BDSRA Foundation’s Annual Family Conference, is part of a broader initiative to improve patient outcomes and support families impacted by Batten diseases. URBC is one of only five institutions named by the organization as a Center of Excellence and is part of the newly established University of Rochester Golisano Intellectual and Developmental Disabilities Institute.
“This recognition underscores our commitment to providing comprehensive care to patients and their families while advancing critical research,” said pediatric neurologist Jennifer Vermilion, MD, director of the URBC. “With this support, we will continue our efforts to develop new therapies and improve the quality of life for those affected by Batten diseases.”
URBC offers a multidisciplinary approach to treating Batten diseases, ensuring that patients receive coordinated care from a team of specialists. The clinical team includes neurologists, geneticists, ophthalmologists, neuropsychologists, and other healthcare professionals who work together to address the complex needs of Batten patients and their families.
Read More: URMC Named Batten Disease Center of ExcellenceNasir Uddin Receives DP1 Grant to Study Liver Disease and Brain Health in People Living with HIV
Monday, July 8, 2024
 A new $2.7 million Director’s Pioneer Award (DP1) grant from the National Institute Diabetes and Digestive and Kidney Diseases (NIDDK) has been awarded to Nasir Uddin, PhD, to study how non-alcoholic fatty liver disease (NAFLD) impacts brain function in people living with HIV. Despite advancements in antiretroviral therapy, liver-related health issues remain a significant concern, with NAFLD affecting up to 50 percent of this population.
A new $2.7 million Director’s Pioneer Award (DP1) grant from the National Institute Diabetes and Digestive and Kidney Diseases (NIDDK) has been awarded to Nasir Uddin, PhD, to study how non-alcoholic fatty liver disease (NAFLD) impacts brain function in people living with HIV. Despite advancements in antiretroviral therapy, liver-related health issues remain a significant concern, with NAFLD affecting up to 50 percent of this population.
The study will explore the combined effects of NAFLD and HIV on brain health. Researchers believe that individuals with both conditions may suffer from more severe brain injury and cognitive impairments due to persistent blood-brain barrier dysfunction, metabolic issues, and microcirculation changes, especially as they age. This study aims to shed light on these complex interactions and uncover new insights into the progression of brain injuries associated with NAFLD in people living with HIV.
To achieve this, Uddin's team will develop a fast, non-invasive molecular MRI method using compressed sensing and artificial intelligence, enabling precise measurement of metabolic dysfunction in the brain with high accuracy. Alongside this new method, they will use advanced MRI techniques and deep learning models to evaluate the impact of NAFLD on cognitive performance, with the goal of improving our understanding of NAFLD-associated brain injury and disease progression. This research could have broader implications for other brain-related disorders, potentially leading to improved diagnostic and therapeutic strategies.
Uddin expressed his enthusiasm for the project, stating, "This grant provides us with an incredible opportunity to explore the complex relationship between liver disease, HIV infection, and their neurological implications,” said Uddin. “We are optimistic that our research will lead to new insights and a comprehensive understanding of brain health in the context of coexisting disorders like liver disease and HIV."
Study Reveals Brain Fluid Dynamics as Key to Migraine Mysteries, New Therapies
Friday, July 5, 2024
New research describes for the first time how a spreading wave of disruption and the flow of fluid in the brain triggers headaches, detailing the connection between the neurological symptoms associated with aura and the migraine that follows. The study also identifies new proteins that could be responsible for headaches and may serve as foundation for new migraine drugs.
“In this study, we describe the interaction between the central and peripheral nervous system brought about by increased concentrations of proteins released in the brain during an episode of spreading depolarization, a phenomenon responsible for the aura associated with migraines,” said Maiken Nedergaard, MD, DMSc, co-director of the University of Rochester Center for Translational Neuromedicine and lead author of the new study, which appears in the journal Science. “These findings provide us with a host of new targets to suppress sensory nerve activation to prevent and treat migraines and strengthen existing therapies.”
Read More: Study Reveals Brain Fluid Dynamics as Key to Migraine Mysteries, New TherapiesNew Art Space in Neurology Embraces Diversity and Equity
Thursday, May 2, 2024

The Department of Neurology has opened the doors on a new art gallery that will feature diverse artistic voices. Under the stewardship of noted Rochester artist Shawn Dunwoody, the Unity Gallery will leverage art to provoke thought, encourage dialogue, and celebrate the voices, minds, and faces that shape the community and medicine.
“The population of the United States is not adequately represented in the field of medicine,” said Blanca Valdovinos, MD, associate chair of Diversity, Equity, Inclusion, and Justice for the Department who helped lead efforts to create the new gallery. “The Unity Gallery is designed to be a focal point where faculty, staff, residents, and visitors encounter a visual narrative that embodies the inclusivity and diversity integral to the Department's identity and represents the commitment to creating an environment where everyone feels a sense of belonging.”
The Unity Gallery is in Department of Neurology’s Joynt Corridor located in 5.4300 in Strong Memorial Hospital and is open to visitors from 11:00 AM to 4:00 PM on weekdays. The works can also be viewed virtually on the Unity Gallery website.
“Art opens ourselves up to more perspectives, to more cultures, broader ways of thinking about things, and it can build critical thinking skills,” said Bob Holloway, MD, MPH, chair of the Department of Neurology. “Art can build empathy with people, and those are very humanistic traits that not only make us better people, but it can also make us better physicians. Our primary job is to make people feel seen, feel heard, understand their perspectives, walk in their shoes, and then we can partner with them better.”
Read More: New Art Space in Neurology Embraces Diversity and EquityMaiken Nedergaard receives Nakasone Award
Wednesday, May 1, 2024

Maiken Nedergaard, a professor of neurology, has been recognized by the International Human Frontier Science Program Organization with its 2024 Nakasone Award for her “groundbreaking discovery and exploration” of the glymphatic system, the brain’s unique waste removal system, and the role that sleep plays in its function.
Nedergaard is codirector of the Center for Translational Neuromedicine, which maintains research facilities at the University of Rochester Medical Center and the University of Copenhagen. In 2012, her lab first described the glymphatic system, a previously unknown network of channels that piggybacks on blood vessels. The system is used to transport cerebrospinal fluid deep into brain tissue and flush away toxic waste, including beta amyloid and tau, two proteins associated with Alzheimer’s disease.
David Gill to Lead Cognitive and Behavioral Neurology
Monday, April 1, 2024

David Gill, MD, has been appointed chief of the Division of Cognitive and Behavioral Neurology at the University of Rochester Medical Center (URMC). A highly respected local clinician and academic, Gill returns to the institution where he completed his residency and fellowship training and assumes his new position effective April 1, 2024.
‘Working in collaboration with our colleagues in Psychiatry, Dave has an exciting vision for the future of dementia care in our community,” said Robert Holloway, MD, MPA, chair of URMC Department of Neurology. “He will help grow the Memory Care Program, improve access to cutting-edge treatments for patients and families in a socially responsible manner, and expand training opportunities to increase the numbers of providers that care for patients with cognitive disorders, specifically in the Rochester area.”
Gill will work with the teams in the Alzheimer’s Disease Care, Research and Education (AD-CARE) Program, the Del Monte Neurosciences Institute, and the University of Rochester Aging Institute to support and help grow basic science and clinical research programs in the field of cognitive disorders. Gill will also build upon his existing relationships in the community to advance education for patients and caregivers through partnerships with Lifespan, the Alzheimer’s Association, and other community groups.
Read More: David Gill to Lead Cognitive and Behavioral NeurologyJamie Capal Tapped as New Head of Child Neurology
Friday, February 9, 2024
 Jamie Capal, MD, has been selected the next chief of the Division of Child Neurology at the University of Rochester Medical Center (URMC) and Golisano Children’s Hospital. Capal—who specializes in intellectual and developmental disabilities—joins a program that has, though more than 50 years of clinical innovation and research, transformed care for children with neurological disorders.
Jamie Capal, MD, has been selected the next chief of the Division of Child Neurology at the University of Rochester Medical Center (URMC) and Golisano Children’s Hospital. Capal—who specializes in intellectual and developmental disabilities—joins a program that has, though more than 50 years of clinical innovation and research, transformed care for children with neurological disorders.
“Jamie has an exciting vision to lead our pre-eminent program in Child Neurology to even greater heights,” said Bob Holloway, MD, MPH, chair of the Department of Neurology. “She will use her prior experiences to mentor faculty, providers, trainees, and staff to build and support successful teams around the many priority programs within the division and across the Medical Center. She will also play an instrumental role in intellectual and developmental disabilities research and the growth of our rare disease and gene therapy clinical trials operations.”
Capal will hold the Frederick A. Horner, MD, Endowed Distinguished Professorship in Pediatric Neurology and will also have an appointment in the Department of Pediatrics. She will also serve as co-director of the Human Clinical Phenotyping and Recruitment Core of the University of Rochester Intellectual Developmental Disability Research Center (UR-IDDRC). She will start her new position on July 1, 2024
“Intellectual and development disabilities are one of the cornerstones of the University’s neuroscience research enterprise, and we are only one of a handful of institutions that hold the three major federally-funded centers of excellence in research, training, care, and community partnership in this field,” said John Foxe, PhD, director of the University of Rochester Del Monte Institute for Neuroscience and co-director of the UR-IDDRC. “These are some of the most complex and challenging diseases in all of medicine, and Dr. Capal’s clinical research experience will enable us to continue to build bridges between the research and clinical programs, and ultimately improve care.”
Read More: Jamie Capal Tapped as New Head of Child NeurologyCalcium Channel Blockers Key to Reversing Myotonic Dystrophy Muscle Weakness, Study Finds
Tuesday, January 2, 2024
 New research has identified the specific biological mechanism behind the muscle dysfunction found in myotonic dystrophy type 1 (DM1) and further shows that calcium channel blockers can reverse these symptoms in animal models of the disease. The researchers believe this class of drugs, widely used to treat a number of cardiovascular diseases, hold promise as a future treatment for DM1.
New research has identified the specific biological mechanism behind the muscle dysfunction found in myotonic dystrophy type 1 (DM1) and further shows that calcium channel blockers can reverse these symptoms in animal models of the disease. The researchers believe this class of drugs, widely used to treat a number of cardiovascular diseases, hold promise as a future treatment for DM1.
“The main finding of our study is that combined calcium and chloride channelopathy is highly deleterious and plays a central role in the function impairment of muscle found in the disease,” said John Lueck, PhD, an assistant professor at the University of Rochester Medical Center (URMC) in the Departments of Pharmacology and Physiology, and Neurology. “Our research also suggests that muscle impairment in DM1 is potentially mitigated by common clinically available calcium channel blockers and that calcium channel modulation is a potential therapeutic strategy.” Lueck is lead author of the study, which appears in the Journal of Clinical Investigation.
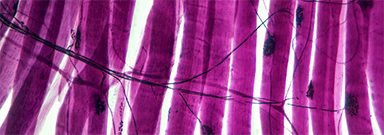
Toxic RNA disrupts muscle function
Myotonic dystrophy is one of the most common forms of muscular dystrophy. People with the disease have muscle weakness and prolonged muscle tensing (myotonia), making it difficult to relax muscles after use. The disease also affects the eyes, heart, and brain, leading eventually to difficulty walking, swallowing, and breathing.
More than 20 years ago, URMC neurologist Charles Thornton, MD, and others uncovered how a genetic flaw–a trinucleotide repeat expansion that results in thousands of repetitions of code on a segment of chromosome 19–gives rise to DM1. This repeat expansion, which grows longer over time, results in the creation of abnormal RNA which accumulates in the nucleus of cells and interferes with the normal processing of many other RNAs. Thornton is a co-author of the current study and the research was a collaboration between the Lueck and Thornton labs.
Read More: Calcium Channel Blockers Key to Reversing Myotonic Dystrophy Muscle Weakness, Study FindsResident Interviews
Monday, January 1, 2024
The Department of Neurology would like to welcome residency applicants, interviewing on Monday, January 8th
Child Neurology Applicants
Naomi Cohen – The University of Texas Southwestern Medical School
Micailya Hall – Eastern Virginia Medical School
Melissa Huberman – University of Miami
Lucy Laura Olivieri – University of New England
Adryanna Tucker – Edward Via College of Osteopathic Medicine