News
Workshop on JNCL Clinical Trials Outcomes
Wednesday, December 18, 2013

There are a number of recent and ongoing clinical trials in Batten Disease. Most of these are focused on asking if these potential new treatments are safe. After safety studies are completed, the next stage of clinical trials research is to learn if these or other interventions are effective. In order to answer this question, we will need a way to measure whether or not an intervention actually makes a meaningful difference in disease course.
Therefore, the URBC hosted a workshop titled, Outcome Measures and Infrastructure for Phase III Studies in JNCL (December 6-7, 2013). The workshop brought together experts in the clinical features of JNCL, experts from other fields (clinical trials in rare diseases, statistics, etc.), and Batten family representatives. Each expert was invited to bring trainee to accompany him/her, so that we can continue cultivating the next generation of researchers who are focused on Batten Disease. Our goals were to:
- Identify possible outcome measures for future clinical trials
- Develop a roadmap for further research to test and refine outcome measures
- Strengthen research collaborations to support outcome measure development
Film Screening and Q&A on Huntington's Disease
Wednesday, December 11, 2013
There will be a film screening of the documentary Alive & Well followed by a Q&A with Kevin Biglan, neurologist and codirector of the Huntington's Disease Society of America Center of Excellence at the Medical Center. The screening starts at 7 p.m. Monday, Dec. 16 at the Little Theatre. Biglan will be joined by Billy Lawler, a former Rochester police officer and founder of Bill Lawler Annual Huntington's 5K. View the film trailer and purchase tickets in advance.
Jones Memorial and URMC Expand Neurology and Cardiology Services
Tuesday, December 10, 2013
Jones Memorial Hospital is expanding its collaboration with the University of Rochester Medical Center through new neurology and cardiology services in Wellsville, NY. URMC neurologists Richard Welles, M.D. and Su Kanchana, M.D., Ph.D., and internist Linda Welles, M.D. began seeing patients at the hospital beginning December 3.
Richard Welles is board certified in Psychiatry, Neurology, and Electrodiagnostic Medicine, and will offer on-site evaluation and treatment of neurological disorders. Kanchana is board certified in Psychiatry and Neurology, and specializes in treatment of adult movement disorders such as Parkinson's disease. Linda Welles is board certified in Internal Medicine and Geriatrics and specializes in gait and balance and geriatric disorders.
We are very pleased to be able to offer neurological care to patients in Wellsville and beyond,
said Eva Benedict, CEO of Jones Memorial Hospital. This collaboration between Jones Memorial and URMC will enable patients to access the necessary specialized care right here in our own community.
Kieburtz Named AAAS Fellow
Tuesday, December 10, 2013

Kieburtz, M.D.
Karl Kieburtz, M.D., M.P.H. has been named a fellow of the American Association for the Advancement of Science (AAAS). Kieburtz, the Robert J. Joynt Professor in Neurology, serves as director of the University of Rochester Medical Center's Clinical and Translational Science Institute and the Center for Human Experimental Therapy.
AAAS is the world's largest and most prestigious scientific society and publishes the highly-regarded
scientific journal Science. Fellows are elected annually by the AAAS for efforts on behalf of
the advancement of science or its applications [which] are scientifically or socially distinguished.
The new Fellows will be
recognized at the AAAS annual meeting in Chicago in February 2014.
Telemedicine Brings Parkinson’s Care to Anyone, Anywhere
Wednesday, December 4, 2013
A new study shows that a neurologist in an office thousands of miles away can deliver effective specialized care to people with Parkinson’s disease. For individuals with the condition – many of whom have never seen a specialist – these virtual house calls
could allow them to live independently while effectively managing the symptoms of the disease.
The idea that we can provide care to individuals with Parkinson’s disease regardless of where they live is both a simple and revolutionary concept,
said University of Rochester Medical Center (URMC) neurologist Ray Dorsey, M.D., M.B.A., senior author of the study which appears today in the journal Neurology: Clinical Practice. This study demonstrates that, by employing essentially the same technology that grandparents use to talk to their grandchildren, we can expand access to the specialized care that we know will improve patients’ quality of life and health.
URMC Plays Role in New Epilepsy Technology
Monday, December 2, 2013
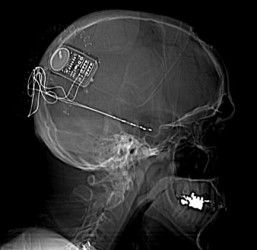
Physicians at the University of Rochester Medical Center (URMC) Strong Epilepsy Center were involved in the recent approval of a new treatment for epilepsy. The implantable medical device - called the Responsive Neurostimulator System (RNS) - monitors brain activity and can detect and counteract seizures.
URMC was one of only 28 sites in the country to conduct clinical trials of RNS, which was developed by the California-based company Neuropace. The research showed that the device decreases the number of monthly seizures by nearly 38 percent. URMC neurologists Michel Berg, M.D. and James Fessler, M.D., and neurosurgeon Web Pilcher, M.D., Ph.D. were involved in the study.
This is the first FDA-approved brain implant for epilepsy that responds to the brain's activity,
said Berg, an associate professor of Neurology. For patients who are unable to control their seizures with medications or are not eligible for resective surgery, this device could provide an important treatment option.
Neurology for the Primary Care Provider
Wednesday, November 27, 2013
The continuing medical education activity Neurology for the Primary Care Provider is scheduled for Thursday, Dec. 12. The program highlights the most recent diagnostic and treatment advances in the field of neurology. The conference runs from 8:30 a.m. to 4:15 p.m. in the School of Medicine and Dentistry.
Now it its twentieth year, Neurology for the Primary Care Provider continues to attract a large audience of clinicians who manage patients with acute and chronic neurologic disorders in diverse settings. Each year, over 100 health care professionals - approximately one half of whom are physicians - attend this conference. The program highlights the most recent diagnostic and treatment advances in the field of neurology, utilizing a highly interactive case-based format.
Drug Shows Early Promise in Treating Liver Failure-Related Seizures
Sunday, November 17, 2013

A study out today in the journal Nature Medicine suggests a potential new treatment for the seizures that often plague children with genetic metabolic disorders and individuals undergoing liver failure. The discovery hinges on a new understanding of the complex molecular chain reaction that occurs when the brain is exposed to too much ammonia.
The study shows that elevated levels of ammonia in the blood overwhelm the brain's defenses, ultimately causing nerve cells to become overexcited. The researchers have also discovered that bumetanide - a diuretic drug used to treat high blood pressure - can restore normal electrical activity in the brains of mice with the condition and prevent seizures.
Ammonia is a ubiquitous waste product of regular protein metabolism, but it can accumulate in toxic levels
in individuals with metabolic disorders,
said
Maiken Nedergaard, M.D., D.M.Sc.,
co-director of the University of Rochester Medical Center (URMC)
Center for Translational Neuromedicine and lead author of the
article. It appears that the key to preventing the debilitating neurological effects of ammonia toxicity is to correct a molecular malfunction which causes nerve cells in the brain to become chemically unbalanced.
Clinical Trial for Children with Juvenile Neuronal Ceroid Lipofuscinosis (JNCL)
Friday, November 1, 2013
The University of Rochester Medical Center is currently recruiting subjects with JNCL for a clinical trial. This research study will focus on evaluating whether an investigational drug is safe and well tolerated in children with JNCL. Mycophenolate mofetil (also known as Cellcept) is a medication that suppresses the immune system. The study is 22 weeks long with a total of 8 in-person visits and 4 telephone contacts. Four visits require travel to University of Rochester Medical Center in Rochester, New York, and four visits are with your child’s local physician. Four contacts take place by telephone. Travel costs are covered by the study. Children enrolled in the study will take mycophenolate syrup twice a day, and will have blood drawn at each study visit to monitor safety.
More information on the trial can be found at ClinicalTrials.gov, Time Warner Cable News (Rochester, NY television affiliate) and the URMC Newsroom.
For further information, please contact Amy Vierhile at (585) 275-4762.
URMC Expands Neuromedicine Teams for Rochester, Ithaca, Southern Tier
Tuesday, October 29, 2013
Four neuromedicine specialists have joined the University of Rochester Medical Center, enhancing programs for traumatic injury, cerebrovascular, spine and Parkinson's care.
Manjunath Markandaya, M.B.B.S., was named chief of the division of neurocritical care and assistant professor of Neurosurgery, Neurology and Medicine. He specializes in caring for some of the most challenging and critically ill neurosurgical and neurological patients.
James C. Metcalf Jr., M.D., was named assistant professor of Neurosurgery and serves Cayuga Medical Center in Ithaca. He specializes in spine disorders and cancer care.
Su Kanchana, M.D., Ph.D., a neurologist, was named assistant professor of Neurology and serves patients in the Southern Tier Neuromedicine office in Big Flats as well as in Rochester at 919 Westfall Road, Building C. She specializes in the diagnosis and management of complex movement disorders, with emphasis on Parkinson's disease, deep brain stimulation and Botulinum toxin therapy.
Amrendra Singh Miranpuri, M.D., joined the team as an assistant professor of Neurosurgery. He specializes in open and interventional neurosurgical procedures for cerebrovascular disease. He is also the surgical co-director of the Neuromedicine Critical Care Program.
URMC's neuromedicine programs - Neurosurgery and Neurology - are ranked 29th best in the nation by U.S. News & World Report.
Sleep 'Cleans' the Brain of Toxins
Thursday, October 17, 2013
The US team believe the waste removal system
is one of the fundamental reasons for sleep. Their study, in the journal Science, showed brain cells shrink during sleep to open up the gaps between neurons and allow fluid to wash the brain clean. They also suggest that failing to clear away some toxic proteins may play a role in brain disorders.
One big question for sleep researchers is why do animals sleep at all when it leaves them vulnerable to predators? It has been shown to have a big role in the fixing of memories in the brain and learning, but a team at the University of Rochester Medical Centre believe that housework
may be one of the primary reasons for sleep.
The brain only has limited energy at its disposal and it appears that it must choose between two different functional states - awake and aware or asleep and cleaning up,
said researcher Dr Maiken Nedergaard. You can think of it like having a house party. You can either entertain the guests or clean up the house, but you can't really do both at the same time.
Doctor Left Behind Story in Search of Ending
Wednesday, September 25, 2013
We live in the new age of Sherlock Holmes, what with movie and television versions of Sir Arthur Conan Doyle's moody but brilliant detective popping up like foggy nights in London town.
But it would seem that the late Dr. Robert J. Joynt, the former dean of the University of Rochester School of Medicine and Dentistry and an internationally recognized neurologist, was ahead of the Holmes revival. In addition to his formidable record of academic publication, Joynt, a Pittsford resident who died in April 2012 at age 86, had begun to turn out a series of short stories, five of which were published in Neurology, a medical journal.
Each mystery featured Holmes and his sidekick Dr. Watson confronted with a puzzler that had a solution grounded in neurology, the study of the nervous system. Joynt's sixth, and presumably last, Holmes mystery was found unfinished on his computer after his death.
Now the editors of Neurology are asking readers to complete the neurologist's story in 1,500 words or less. The winning entry will be published in Neurology. The author of the new material will share credit with Joynt. The uncompleted mystery and the contest rules can be found by going to Neurology.org and searching for The Case of the Locked House,
the title of the incomplete story. (When you get to the story, click on Full Text.)
Michael J. Fox Still Pushing to Find Parkinson's Cure
Tuesday, September 24, 2013
Actor Michael J. Fox once predicted that he would be cured of Parkinson disease's long before his 50th birthday. I know I won't have this. I will not have it,
he told Barbara Walters on national television. Now, 52, Fox is far from cured.
In a way, not much has changed in the 15 years since Fox first publicly acknowledged that he had the disease and the 22 years since his diagnosis. Most patients still rely on a medication, levodopa, first tested on Parkinson's the year Fox was born. In other ways and much to Fox's credit, many people say our understanding of the disease has been transformed since his diagnosis, bringing research closer to a cure even as scientists acknowledge that it will be far harder to achieve than they once believed.
Still, the only major new treatment in the last two decades is deep-brain stimulation, in which electrodes are implanted inside the brain to partially override the distorted signals that lead to the disease's tremors, stiffness and slowness. Like L-dopa, it only treats symptoms, and can't slow or stop the disease. Another recent advance, according to Irene Richard, a neurologist at the University of Rochester, is the attention now being paid to the emotional and mental toll of Parkinson's. Roughly half of Parkinson's patients are depressed, likely as a symptom of the condition.
Copper Identified as Culprit in Alzheimer's Disease
Monday, August 19, 2013
Copper appears to be one of the main environmental factors that trigger the onset and enhance the progression of Alzheimer's disease by preventing the clearance and accelerating the accumulation of toxic proteins in the brain. That is the conclusion of a study appearing today in the journal Proceedings of the National Academy of Sciences.
It is clear that, over time, copper's cumulative effect is to impair the systems by which amyloid beta is removed from the brain,
said Rashid Deane, Ph.D., a research professor in the University of Rochester Medical Center Department of Neurosurgery, member of the Center for Translational Neuromedicine, and the lead author of the study. This impairment is one of the key factors that cause the protein to accumulate in the brain and form the plaques that are the hallmark of Alzheimer's disease.
Kieburtz Appointed to Oversee URMC Clinical Research
Friday, August 9, 2013
Karl Kieburtz, M.D., M.P.H. has been tapped to serve as director of the University of Rochester Medical Center (URMC) Clinical and Translational Science Institute (CTSI) and to serve as the senior associate dean for Clinical Research. The appointment will be effective September 1, 2013.
As one of the leading academic experts in the design and operation of clinical trials, Dr. Kieburtz is the obvious choice to build upon the Medical Center’s history as an innovative national leader in the field of experimental therapeutics and translational medicine,
said Mark Taubman, M.D., dean of the URMC School of Medicine and Dentistry. We are deeply grateful that he has accepted this new leadership role and I look forward to working with him to continue to strengthen and grow our clinical research enterprise.
New Neurology Appointments to Focus on Expanding Access at Home and Abroad
Thursday, August 1, 2013
Gretchen Birbeck, M.D., M.P.H., and E. Ray Dorsey, M.D., M.B.A., have joined the University of Rochester Medical Center (URMC) Department of Neurology effective August 1. Birbeck, an epilepsy specialist, and Dorsey, a movement disorders specialist, will both focus on the global burden of neurological disorders and efforts to expand access to underserved populations.
The number of people with neurological disorders will grow at a rapid pace over the next several decades,
said Robert G. Holloway, Jr., M.D., M.P.H., chair of the URMC Department of Neurology. Expanding access to specialized care to patients in both the U.S. and the developing world will be one of the key challenges facing medicine. Drs. Birbeck and Dorsey are leaders and innovators in this field and we are thrilled to have them join our department.
Holloway Appointed New Chair of Neurology
Thursday, July 25, 2013

Robert G. Holloway, Jr., M.D., M.P.H. has been tapped as the next chair of the University of Rochester Medical Center (URMC) Department of Neurology. Holloway had been serving as interim chair of the department since last July and his permanent appointment is effective immediately.
Dr. Holloway is the epitome of the academic 'triple threat,'
said Mark Taubman, M.D., dean of the University of Rochester School of Medicine and Dentistry. His skills as a physician, researcher, and educator will enable the department to grow and meet the twin challenges of health care reform and an increasingly competitive national environment for research funding. Bob has played an integral role in many of the Medical Center's signature initiatives and I am deeply grateful that he has agreed to take on this new responsibility and lead the Department of Neurology.
In addition to his position in Neurology, Holloway is also a professor of Public Health Sciences, director of the Research, Education, and Career Development Function of the URMC Clinical and Translational Science Institute (CTSI), and principal investigator of the URMC's NIH-funded NeuroNEXT clinical research program.
Neurology and Neurosurgery Ranked as One of Best in Nation
Tuesday, July 16, 2013

Chair of Neurology, Robert Holloway, Jr., M.D., M.P.H. and Chair of Neurosurgery, Webster H. Pilcher, M.D., Ph.D.
When US News & World Report's 2014 Best Hospitals guidebook hits newsstands today, a record number of six University of Rochester Medical Center specialties will be ranked among the very best in the nation. That's the highest number of URMC programs ever to earn a seat in the magazine's list of the nation's top 50 in a single year, since US News began ranking hospitals in 1989.
The URMC adult specialties nationally ranked included Neurology and Neurosurgery as the 29th best. URMC's success in the U.S. News rankings reflects the hard work that our faculty and staff have invested to continuously improve quality, patient safety and satisfaction. It also reflects URMC's growing reputation for first-rate care,
said URMC CEO Bradford C. Berk, M.D., Ph.D.
Profile of Excellence: Unit 5-1600 Team Pioneers in Providing Exceptional Care to Patients and Families
Sunday, June 30, 2013

For their commitment to patient safety and satisfaction, the nursing staff in the Neurology Inpatient Unit (5-1600) received a 2012 Board Excellence Award in the team category.
A key to the team's success has been their relentless focus on improving communication - both
among caregivers and with patients and their families. This goes far beyond the routine communication
between residents, attending physicians, and nurses as they hand off care during a shift change, to
include hourly huddles
among nursing staff to review patient status, and regular rounding by
nursing staff to check with patients and their families, ensuring that all of their needs are being met.
And, at the prodding of the nursing staff, attending physicians now round at a consistent time each
morning, so the families can plan to participate. Once daily, too, the unit's nurses, therapists,
social workers, and residents all come together to plan the day and develop comprehensive discharge
plans for patients leaving the hospital.
Our unit is home to one of the most challenging patient populations in the hospital, and
delivering timely and effective care requires a multidisciplinary team effort,
said
Todd Holmquist, M.D.,
the medical director of the Neurology Inpatient Unit. This requires cohesion, leadership,
accountability, and - above all - constant communication among providers.
Brain's 'Garbage Truck' May Hold Key to Treating Alzheimer's and Other Disorders
Thursday, June 27, 2013

In a perspective piece appearing today in the journal Science, researchers at University of Rochester Medical Center point to a newly discovered system by which the brain removes waste as a potentially powerful new tool to treat neurological disorders like Alzheimer's disease. In fact, scientists believe that some of these conditions may arise when the system is not doing its job properly.
Essentially all neurodegenerative diseases are associated with the accumulation of cellular waste products,
said Maiken Nedergaard, M.D., D.M.Sc., co-director of the URMC Center for Translational Neuromedicine and author of the article. Understanding and ultimately discovering how to modulate the brain's system for removing toxic waste could point to new ways to treat these diseases.
The body defends the brain like a fortress and rings it with a complex system of gateways that control which molecules can enter and exit. While this blood-brain barrier
was first described in the late 1800s, scientists are only now just beginning to understand the dynamics of how these mechanisms function. In fact, the complex network of waste removal, which researchers have dubbed the glymphatic system, was only first disclosed by URMC scientists last August in the journal Science Translational Medicine.
Neurologists Win Provost’s Multidisciplinary Award
Friday, June 14, 2013
Five diverse research projects at the University were selected as recipients of the sixth annual Provost's Multidisciplinary Awards. The initiative provides $250,000 each year to support faculty research that crosses disciplines. Among the recipients were Neurology professors, Jonathan Mink and Marc Schieber. Their project, entitled, Task-Specific Dystonia in Musicians is a collaboration with Ralph Manchester, in Medicine and Nicholas Goluses (Strings) and Peter Kurau (Woodwind, Brass & Percussion) at the Eastman School of Music.
Huntington's Brain Cells Regenerated, in Mice
Thursday, June 6, 2013
Huntington's disease, like other neurodegenerative diseases such as Parkinson's, is characterized by the loss of a particular type of brain cell. This cell type has been regenerated in a mouse model of the disease, in a study led by University of Rochester Medical Center scientists.
Mice whose received this brain regeneration treatment lived far longer than untreated mice. The study was published online Thursday in Cell Stem Cell.
We believe that our data suggest the feasibility of this process as a viable therapeutic strategy for Huntington's disease,
said senior study author Steve Goldman, co-director of Rochester's Center for Translational Neuromedicine, in a press release.
Researchers Identify Genetic Signature of Deadly Brain Cancer
Monday, June 3, 2013

A multi-institutional team of researchers have pinpointed the genetic traits of the cells that give rise to gliomas -- the most common form of malignant brain cancer. The findings, which appear in the journal Cell Reports, provide scientists with rich new potential set of targets to treat the disease.
This study identifies a core set of genes and pathways that are dysregulated during both the early and late stages of tumor progression," said University of Rochester Medical Center neurologist Steven Goldman, M.D., Ph.D., the senior author of the study and co-director of the Center for Translational Neuromedicine. "By virtue of their marked difference from normal cells, these genes appear to comprise a promising set of targets for therapeutic intervention.
URMC Honored for Stroke, Cardiac Programs
Tuesday, May 28, 2013
The American Heart Association/American Stroke Association (AHA/ASA) has once again recognized the University of Rochester Medical Center's (URMC) Strong Memorial Hospital as having met its highest standards of care for stroke, heart failure, and resuscitation.
This is the fourth consecutive year that Strong Memorial Hospital has received the AHA/ASA Get With The Guidelines program's highest honor, the Stroke Gold Plus Quality Achievement Award. The hospital was also tapped for the Target: Stroke Honor Role, which recognizes hospitals that have consistently and successfully reduced door-to-needle time -- the window of time between a stroke victim's arrival at the hospital, the diagnosis of an acute ischemic stroke, and the administration of the clot-busting drug tPA.
"This recognition is a testament to the hard work of our outstanding team of nurses, physicians, and therapists and their dedication to provide the highest quality of care to stroke victims," said URMC neurologist Curtis Benesch, M.D., Ph.D., the director of the Strong Stroke and Cerebrovascular Center.
Symposium Aims to Get Parkinson's Community Moving
Monday, May 13, 2013
URMC neurologists are participating in a daylong symposium that brings together local Parkinson's disease patients and nationally recognized movement disorders researchers, clinicians, and physical therapists to discuss the latest advances in research and treatment for the disease.
The symposium will be held on Saturday, May 18, 2013 from 10:00 AM to 4:15 PM at the Radisson Rochester Riverside Hotel. The event is free and open to the public.
"The Victory Summit is a fantastic opportunity to share the many ways in which individuals with Parkinson's can alter the course of the disease," said Michelle Burack, M.D., Ph.D., assistant professor in the URMC Departments of Neurology and Pediatrics. Things like daily physical activity, paying attention to mental well-being, and maintaining social connectedness are powerful 'medicine' for the brain, and are vital components of optimum management for this chronic condition.
Vietnam Veterans Could Hold Clue to Future for Today’s Soldiers
Thursday, April 25, 2013
Since 2001, more than two million service members have been deployed in Iraq and Afghanistan, and studies indicate nearly a third of them have suffered traumatic brain injury (TBI), post-traumatic stress disorder (PTSD), or both. The University of Rochester Medical Center is part of an investigation into whether these injuries put the soldiers at greater risk for a future battle -- against Alzheimer’s Disease. As they begin the study, researchers are turning to veterans of the Vietnam War for help.
"In order to predict what might happen, we wanted to look at a cohort that is about 40 years older to see what the brains of those individuals look like," says Anton P. Porsteinsson, M.D., who is overseeing the study at URMC. "Nobody paid much attention to this back in the Vietnam era, but do TBI and PTSD impact your risk of memory disease? Could this point toward additional studies into treatment and prevention of the long-term effects of these injuries?"