Impact Of Various Bariatric Procedures In Treating Diabetes In Menopause
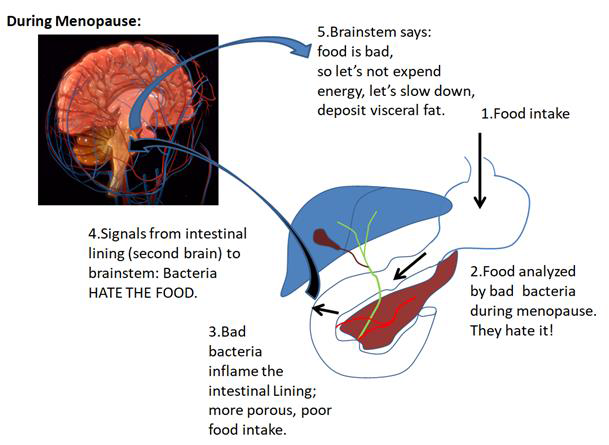
 Weight control challenges many women entering menopause. For some, weight gain is only an assault on their personal image. For others, however, their abdominal obesity more so than their total weight gain significantly increases their risk for type 2 diabetes mellitus and heart disease. Diet and exercise have been the tools for managing weight gain in the past. While effective for some, a more aggressive approach involving bariatric surgery to limit intestinal absorption has been required for those whose body mass index (BMI) places them in the obese category.
Weight control challenges many women entering menopause. For some, weight gain is only an assault on their personal image. For others, however, their abdominal obesity more so than their total weight gain significantly increases their risk for type 2 diabetes mellitus and heart disease. Diet and exercise have been the tools for managing weight gain in the past. While effective for some, a more aggressive approach involving bariatric surgery to limit intestinal absorption has been required for those whose body mass index (BMI) places them in the obese category.
There are a number of types of bariatric surgeries designed to reduce weight. Restrictive procedures such as the laparoscopic adjustable gastric banding (LAGB) and vertical banded gastroplasty (VBG) reduce the volume of food in the stomach in order to decrease caloric intake and reduce one’s appetite. In contrast, malabsorptive procedures like the biliopancreatic diversion (BPD) shorten the small intestine to decrease absorption of nutrients, while combined procedures like the Roux‐en‐Y gastric bypass (RYGB) restrict the stomach volume and also alter the small intestine to decrease absorption.
Historically, bariatric surgery was credited with reducing one’s BMI by restricting caloric intake and, in some patients, improving their diabetes mellitus, an important secondary benefit since nearly 30% of patients undergoing bariatric surgery have type 2 Diabetes. More recently, investigators have noted that certain restrictive bariatric procedures result in rapid resolution or improvement in diabetes within days of the operation, long before the blood glucose improvement could be attributed to weight loss alone. It seems that bariatric procedures that alter absorption in the small intestine affect the peptides within the gut that control insulin secretion, a phenomenon that is not seen following restrictive procedures.
The epithelium of our intestinal tract contains specialized K and L cells (named before their functions were understood) that secrete critical peptides to communicate to our pancreas how to respond to the stimulatory effects of glucose. Glucagon‐like peptide‐1 (GLP‐1) from the L cells of the distal ileum stimulates the pancreatic islets to increase glucose‐dependent insulin secretion, slow gastric emptying to control postprandial glycemia, and increase satiety (a sense of fullness). Glucosedependent insulinotropic peptide (GIP) from the K cells of the proximal gut responds to carbohydrates and fats. Peptide YY (PYY), secreted by L cells of the distal intestine, increases satiety and delays gastric emptying. Ghrelin from the gastric fundus and small intestine regulates appetite in the hypothalamus through increased blood levels before meals and decreased levels after meals.
Two current theories exist to explain this bariatric‐diabetic phenomenon. In the “lower intestinal hypothesis” by Cummings (2007), rapid delivery of nutrients to the distal bowel improves glucose metabolism by increasing secretion of GLP‐1 and other appetite suppressive gut peptides. The “foregut exclusion theory” of Rubino (2008) instead suggests that bypassing the duodenum and proximal jejunum blocks the secretion of a “signal” that promotes insulin resistance.
While the physiology of this remarkable link between certain bariatric procedures and the rapid improvement in type 2 diabetes mellitus remains to be resolved, the observation itself has made investigators in diabetes management go back to the drawing board to rethink old theories and to construct new approaches to care.
By James Woods, M.D.
Dr. Woods treats patients for menopause at the Hess/Woods Gynecology Practice.
Disclaimer: The information included on this site is for general educational purposes only. It is neither intended nor implied to be a substitute for or form of patient specific medical advice and cannot be used for clinical management of specific patients. Our responses to questions submitted are based solely on information provided by the submitting institution. No information has been obtained from any actual patient, and no physician‐patient relationship is intended or implied by our response. This site is for general information purposes only. Practitioners seeking guidance regarding the management of any actual patient should consult with another practitioner willing and able to provide patient specific advice. Our response should also not be relied upon for legal defense, and does not imply any agreement on our part to act in a legal defense capacity.
James Woods | 8/8/2014