Menopause or Menopause Transition: When Does the Cardiovascular Risk Begin?
Your Menopause Question: Menopause or Menopause Transition: When Does the Cardiovascular Risk Begin?
Our Response: Does menopause really begin only after a woman experiences her last menstrual period? On average, the age of these women is 51 years. But, ask any woman in menopause how she recalls the three to five years before she reached that milestone and most will remember that their menstrual cycles became more erratic and unpredictable. We now know that other biological changes also are beginning to occur. In fact, the risks from cardiovascular disease start earlier than initially thought, making this time in life a true challenge for public health interventions. Cardiovascular disease is the leading cause of death in women. But, ask any woman what her greatest fear is, and many would say “breast cancer.” Do we need to refocus? Let’s look at this time in a woman’s life through the lens of biology.
The official statement of the North American Menopause Society (Harlow, 2012) marks the menopause transition as a several‐year window. It begins in late productive years as menses encounters variable lengths. This period is signaled by fluctuating follicle‐stimulating hormone (FSH) levels as declining estrogens from the ovaries fail to produce a negative feedback to the brain. A late menopause transition period of one to three years is marked by consistently rising FSH levels as estrogen levels fall further, followed by early menopause that lasts for two to six years during which FSH levels stabilize at a high level into late menopause (Lobo, 2008). But, what has this to do with the risks that women experience in this chapter of their lives? For those answers, we must examine the critical relationship that exists between estrogen and inflammation.
In the reproductive years, estradiol, 95% of which is produced by the ovaries, functions as the most powerful of the estrogen family. It was always respected for its role in pregnancy and menstrual cycling. Yet, more recently, scientists have shown that during those years estradiol also serves to suppress production of critical inflammatory proteins such as
interlukin 1 (IL‐ 1), interlukin 6 (IL‐6), and tumor necrosis factor alpha (TNF a), which are normally generated by monocytes, macrophages, neutrophils, and other cell populations. These inflammatory proteins, when expressed, are capable of stimulating over 60 other inflammatory proteins that we now recognize attack brain, bone, heart, skin, and blood vessels. The appearance of these inflammatory proteins parallels the fluctuating and then rapidly declining estrogen levels seen in late menopause transition (Hanauer, 2005, and Kredel, 2014).
Women may recognize this period of their lives only by the onset of irregular menstrual periods. Yet, it is during this window of time that estrogen levels fluctuate and even may increase briefly before beginning to decline permanently. It is also a time when some women, for the first time, begin to experience transient hot flashes, mood disorders, vaginal dryness, or sleep disorders. What only now is being appreciated is that this also is a time of increased cardiovascular risk from depression and anxiety.
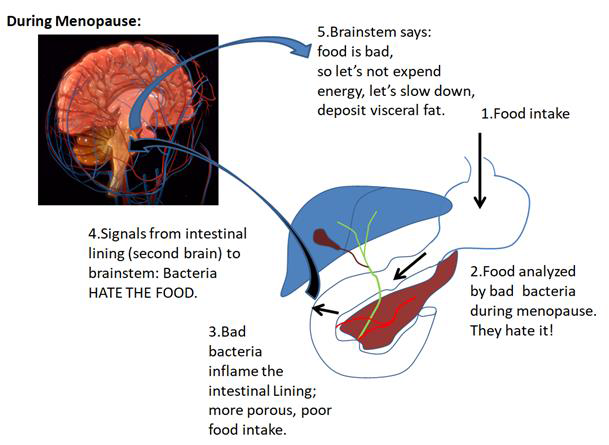
From clinical studies, scientists also have shown that during the three to five years leading up to the last menstrual period, visceral fat that surrounds our abdominal organs and coats our blood vessels increases to a greater degree than does subcutaneous fat (Frayn, 2000, and Shuster, 2012). These specialized fat cells act as tiny factories to produce a wide range of inflammatory proteins. These changes are accompanied by a rise in blood lipid levels and increases in blood vessel wall thickness. These cardiovascular events, while perhaps not generating the emotional reaction of many of the other symptoms, signal the real risk in menopause, that of a cardiovascular event and even stroke.
Yet, emotional changes involving depression and anxiety during the menopause transition, often overlooked by care providers in a gynecology visit, now are emerging as important factors differentiating the cardiovascular risks of younger women from those of women in later menopause. Stated plainly, increasing numbers of studies suggest that young women with coronary heart disease are at greater risk of the adverse cardiovascular effects of psychological stress.
Why would this time in life be so stressful for women? From personal observations from my menopause practice, the list is long. Expectations of life unfulfilled, marriages gone bad, job loss to younger individuals, adult kids with their challenges,
changes in body image, loneliness, and isolation. Are these younger women at greater risk of depression and anxiety than older women or men? In one study of men and women with stable coronary heart disease undergoing myocardial perfusion imaging before and after stress testing, younger women demonstrated greater quantitative and visual indicators of ischemia than men or older women (Vaccarino, 2016). These observations complement studies showing that chronic stress has a greater effect on health than acute stress (Dhabhar, 2014). Witness who in the family assumes responsibility for an older parent?
The importance of these observations adds credibility to the many investigators focusing on the real risks of the menopause transition. It is understandable that discussions in the primary care or gynecology office may address specific symptoms of menopause such as hot flashes, poor sleep, vaginal dryness, weight gain, and loss of libido. But, the real danger is cardiovascular risk in the menopause transition, now emerging as an important target for public health interventions (Samar, 2020).
As scientists continue to clarify the biology and risks of the menopause transition, they will offer education and novel approaches to clinicians and their patients to accommodate this most natural time in life.
James Woods | 12/1/2022