News
November 2020 Publications
Monday, December 14, 2020
- Wendi Cross, PhD was a coauthor on a paper published in Crisis examining the effectiveness of active learning strategies in suicide prevention gatekeeper training.
-
Several members of Psychiatry published a paper in Social Science and Medicine analyzing the perspectives of African American males experiencing civil unrest to determine factors influencing community violence. Racist policies and practices, economic opportunity and mobility, and displays of power in the community impacted escalating violence.
-
Wilfred Pigeon, PhD, alongside Jason DeViva, PhD of Yale School of Medicine, published an editorial expanding on Werner et al.'s research on fear of sleep as a clinically significant construct in trauma and PTSD.
-
Anton Porsteinsson, MD was a coauthor on a paper examining hippocampal volume and cortical thickness in subjects with the Apolipoprotein ε4 allele. There was a correlation between hippocampal volume atrophy and cortical thinning and cognitive change in APOE ε4/ε4 subjects with early Alzheimer's disease.
-
Steven Silverstein, PhD was a coauthor in this review of mental health needs in people with visual impairment. The paper suggest that a better understanding of the mechanisms linking visual impairment with mental health challenges is needed in order to improve the detection and treatment of mental health problems in this population.
-
Catherine Cerulli, JD, PhD was a coauthor on this study using machine learning to analyze social media for the reasons given for staying in/ leaving abusive relationships. The results of the study will provide insight into the dynamics of partner violence.
- Thomas O'Connor, PhD was a co-author in this paper examining the influence of prenatal androgen exposure on children's gender-typed behavior.
- Yeates Conwell, MD was a co-author on an article examining existing research surrounding suicide in individuals with Lewy body dementia.
- Steve Silverstein, PhD was a co-author in a paper published in Psychiatry Research looking at how nicotine affects performance on cognitive tasks.
- Yeates Conwell, MD was a co-author on a paper examining associations between well-being, suicide and self-harm in older adults.
-
Eric Caine, MD was a coauthor in this study examining social media data to analyze people's psychosocial concerns during the COVID-19 pandemic.
Pediatric Behavioral Health and Wellness, Bridge Art Gallery Now Accepting Submissions for "Not a Moment But a Movement" Art Exhibition
Monday, December 14, 2020

Pediatric Behavioral Health & Wellness Outpatient Services' Racial Justice Committee is partnering with The Bridge Art Gallery for their first call for art of 2021! The show, Youth for Racial Justice: Not A Moment But A Movement, is open to all youth under age 21. The deadline for submissions is January 8th, 2021 by emailing the Bridge Art Gallery or by dropping off pieces at Pediatric Behavioral Health & Wellness locations. Please share with anyone you think may be interested in participating!
October 2020 Publications
Thursday, November 12, 2020
- Steven Silverstein, PhD contributed to the investigation of the effects of Parkinson's disease on retinal activity in this study using Flash Electroretinography data parameters from 21 participants as a non-intrusive measure of retinal activity.
- Peter Wyman, PhD, Anthony Pisani, PhD, Lacy M. Morgan-DeVelder, MS, LMFT, Karen Schmeelk-Cone, PhD, and Eric Caine, MD helped evaluate suicide prevention and mental health programs for US Air Force personnel. The Wingman-Connect program studied is the first to reduce suicidal ideation and depression symptoms in a general Air Force population.
- Marsha N. Wittink, MD, MBE completed a qualitative study of community oncologists and older adults with Acute Myeloid Leukemia (AML) to determine influences on initial treatment and transplant decision-making.
- Mark Oldham, MD characterized frequent neuropsychiatric complications relating to COVID-19. Evaluating how inconsistent terminology can place constraints on mental status research/diagnosis, and expressing the importance of shared classification and nomenclature.
- Elizabeth Karras, PhD led a trial focusing on whether firearm safety messaging is related to changes in safe storage intentions and behaviors in US military veterans.
- Mark Oldham, MD was a coauthor on a paper published in Psychosomatics reviewing subtypes of personality changes due to other medical conditions.
- Mark Oldham, MD and Hochang Ben Lee, MD, alongside I?Hsin Lin, PhD, Keith Hawkins, PsyD, Fang?Yong Li, MPH, David Yuh, MD of Yale School of Medicine, published a paper on the relationship between depression and cognitive and functional decline after coronary artery bypass grafts.
Tziporah Rosenberg Named Associate Chair of Education
Wednesday, November 4, 2020
 Tziporah Rosenberg, PhD, LMFT, has been appointed as the new Associate Chair of Education, effective as of January 1st, 2021. In this role, Dr. Rosenberg will lead our overall education and training agenda in the Department of Psychiatry. She succeeds Deborah King, PhD who retired from the role at the end of September.
Tziporah Rosenberg, PhD, LMFT, has been appointed as the new Associate Chair of Education, effective as of January 1st, 2021. In this role, Dr. Rosenberg will lead our overall education and training agenda in the Department of Psychiatry. She succeeds Deborah King, PhD who retired from the role at the end of September.
In addition to serving as an Associate Professor in the Department of Psychiatry and Family Medicine, Rosenberg also currently serves as the Director for Training and Education in our Division of Collaborative Care and Wellness and has been an important member of our leadership team integrating behavioral health across our community's primary care practices. She is also Director of the Institute for the Family's Family Therapy Services and a member of the Behavioral Health Integration Team for Accountable Health Partners, our region's premier integrated network of community and faculty providers and regional hospitals largely affiliated with URMC.
During the extensive search for this important leadership position, Dr. Rosenberg presented a compelling vision for inter-professional training and interdisciplinary education. We are very excited and proud to welcome the new Associate Chair of Education who is a Licensed Marriage and Family Therapist.
Speaking on Dr. Rosenberg, Hochang Ben Lee, MD says, "Her leadership skills in education and training prowess are already well-known across our medical center and beyond."
Dr. Rosenberg comments, " I am looking forward to continuing the tradition of excellence with which Deborah King served in this vital leadership role, and also seeding some possibilities for innovation around interprofessionalism, team-based care, and reinforcing a culture of shared learning among all of our Department's dedicated staff, faculty, and leadership."
Please join us in welcoming and congratulating Dr. Rosenberg in her new role!
Celebrating Deborah King, PhD
Monday, November 2, 2020
September 31st was the last day of work for Deborah King, PhD, our Associate Chair of Education and Chief of Psychology, as she retires after 39 years of service to our department. In her role, she has supported the careers of many trainees and faculty members of all disciplines and background in our department while also providing psychotherapy services.
Speaking on King's leadership, Chair of the Department of Psychiatry Hochang Ben Lee, MD states, "It's hard to imagine our department without Deborah, and vice-versa. She has been so integral to what we are and what we stand for."
A virtual event featuring musical dedications from co-workers was held on October 29th to celebrate Deborah's years if service, mentorship, and friendship.

Thank you for all your years of service, Deborah! We are wishing you the best in this next chapter of your life!
Courtney Blackwood Joins Psychiatry as Director of Nursing
Thursday, October 8, 2020
We are pleased to announce that Courtney Blackwood, MS, RN, NE-BC, has been appointed Director of Nursing for Psychiatry, effective October 19, 2020. In this role, Ms. Blackwood will lead all nursing operations in the Department of Psychiatry for Strong Memorial Hospital for inpatient areas and outpatient areas in the region.Many of you may know Ms. Blackwood from her role as Senior Nurse Manager of the Adult Medical Hematology/Oncology Unit at Wilmot Cancer Center, where she has done an outstanding job of leading the nursing team since beginning the role in 2017. Ms. Blackwood sits on many committees at Wilmot and Strong, including acting as Chair of Cancer Center Safety Rounds. She was instrumental in leading the efforts to launch our new Nurse Manager Residency program. Ms. Blackwood brings ten years of leadership experience to Psychiatry; she took her first assistant nurse manager position in 2011, in the Adult Cardiothoracic, Plastic & Burn Surgery Unit.
Ms. Blackwood graduated with her Bachelor's Degree in Nursing from St. John Fisher in 2009. She began her career as a registered nurse in Adult Inpatient Psychiatry in 2009, at St. Mary's Hospital. Ms. Blackwood held the role of Clinical Adjunct Professor at Monroe Community College, leading nursing students through their clinical rotations in Mental Health at St. Mary's Hospital from 2013 to 2015. She also held the role of Clinical Adjunct Professor at St. John Fisher, leading students through their clinical rotations in Medical Surgical Nursing at Strong from 2012 to 2017. In 2017, Ms. Blackwood graduated with her Master's Degree in Healthcare Management from the University of Rochester and received her Nurse Executive Certification in 2018.
Ms. Blackwood's advocacy for nurses and experience leading teams will serve her well in her new role. Please join us in welcoming and congratulating Courtney Blackwood in her new role as Director of Nursing for Psychiatry.
A special thank you to Keri Cockman for acting as Interim Director of Nursing for Psychiatry while we filled this position.
Ellen Poleshuck Receives Susan McDaniel Collaborative Care Award
Thursday, October 8, 2020
Please join us in congratulating Ellen Poleshuck, PhD on being the 2020 recipient of the Susan McDaniel Collaborative Care Award! This award was started in 2016 to recognize individuals who have demonstrated excellence in promoting the integration of behavioral health and general medical care through clinical work, research or education. She was virtually recognized by Susan McDaniel, PhD during this year's Collaborative Care & Wellness 5th Annual Symposium on October 2, 2020. 
Dr Poleshuck is an Associate Professor of Psychiatry and Obstetrics/Gynecology at the University of Rochester, and serves as Director of the Women's Behavioral Health Service. She is a clinical psychologist and a marriage and family therapist, specializing in the assessment and treatment of underserved women and families who present for care in obstetric and gynecology practices. She also is Clinic Director of Healing Through Education, Advocacy, and Law (HEAL), an innovate multi-disciplinary clinic for people experiencing intimate partner violence. Her research focuses on integrated treatments for women with depression and co-occurring concerns such as pain, partner violence, and socioeconomic disadvantage.
Speaking on her accomplishments, George Nasra, MD says, "Dr. Poleshuck's leadership and her pioneer work in women's health integration and for individuals with trauma and domestic violence are not only innovative but have contributed significantly in promoting health and decreasing disparities in care for our community and the region."
Tziporah Rosenberg, PhD, who works closely with Dr. Poleshuck on our Integrated Care Clinics and is in charge of training staff and clinicians to provide this care, lists her five reasons why she believes Ellen deserves this award. She says:
- Dr Poleshuck has been a tireless leader for women's health across all biopsychosocial domains--through her clinical leadership, program development, and research that has brought her all over the world to learn, teach, and collaborate.
- She is known for her culturally-sensitive mental health care for underserved women and their families.
- She demonstrates her leadership and dedication to integration as a mentor to learners and junior faculty across specialties, institutions, and international borders, particularly those who are invested in clinically-focused, population-level research about mental health issues in vulnerable populations.
- Ellen is a respected scholar with a track record of high impact publications focused on chronic pain, depression, violence, and women's health issues. Her collaborative spirit is demonstrated in part by the fact that the vast majority of her publications are authored with her by teams of other clinicians, researchers, and learners.
- She is a stalwart advocate for evidence-based psychotherapies, and she has translated this focus into her recent work on integrated primary care, using data and measurement to track outcomes at the patient-, practice-, and population levels.
Finally, Kate Cerulli, JD, PhD, who works closely with Poleshuck in developing and studying approaches like the HEAL Clinic, to help women experiencing intimate partner violence. Kate said:
"When we think about Collaborative Care, the two words hold their unique meanings. In terms of collaborating on issues related to intimate partner violence and pain, Ellen was eager to learn why I thought a partnership might be helpful to the survivors I work with at court. She shared her observations of the clients she served, especially their histories of trauma and comorbid health issues. Collaboration is the action of working with someone to produce or create something, and that is exactly what Ellen did. Years later, we had created a community advisory board, sought insight from a patient advisory board, and launched the HEAL Collaborative with community partners. The word Care comes in because at her core -- that is Ellen. If you know Ellen, you know how deeply she cares about all those she meets. She leaves people feeling better than when they first met her."
Please join us in congratulating Dr. Poleshuck on this well-deserved award!
Racial Justice Initiatives Group in Supporting Our Community
Tuesday, October 6, 2020
During times of despair, compassion and empathy are no longer luxuries; they are necessities. This was the exact thought process UR Medicine: Pediatric Behavioral Health and Wellness Outpatient Services' leadership and staff had in mind when developing a new relationship with one of the longest standing organizations in the Rochester community aimed at the educational advancements of our youth of color. The Urban-Suburban Interdistrict Transfer Program began in June of 1963 as a way to decrease racial isolation and enhance opportunities for students living within the Rochester community. Nearly 60 years later, the program has partnered with 16 districts to support cultural diversity in suburban schools.
With racial tension increasing around the country in the wake of several racially charged tragedies, our staff at UR Medicine: Pediatric Behavioral Health and Wellness Outpatient Services stepped up to offer support, and become an ally to our community. With the support of several dedicated team members, the Racial Justice Initiatives Group organized by Linda Alpert-Gillis, Ph.D., and coordinated by Shun Hill, LMHC, Senior Mental Health Therapist and Jerard Johnson, Senior Psychiatric Case Manager have taken on several projects. Brianna Daniels, LMHC a former student of the Urban-Suburban Program, as well as Aliyah Patterson, LMHC opened the doors of communication between the Urban-Suburban Interdistrict Transfer Program and the service. As newly connected community allies, Ms. Daniels has already presented at a parent orientation session for youth attending the Pittsford Central School District, and have other events planned with the parents and youth of the Urban-Suburban Interdistrict Transfer Program. The community conversations planned will include a forum for parents to inquire about services offered in our outpatient service, provide psychoeducation around the importance of mental health well-being in today's youth, and connect families with resources to assist with child and adolescent mental health concerns. In the future the group hopes to expand this alliance to include additional resources and streamline access to care.
ACLP Appoints Hochang Lee, MD as Psychosomatics Editor-in-Chief
Friday, September 18, 2020
Hochang Ben Lee, MD has been appointed as The Academy of Psychosomatic Medicine editor-in-chief for the Academy's Psychosomatics journal. Dr. Lee is assuming the role from Ted Stern, MD, FACLP, the journal's Editor-in-Chief since 2008.
Commenting on his appointment, Dr. Lee says, "I am looking forward to the challenges ahead and the opportunity to make new contributions to the Academy and to the future of [consultation-liason] Psychiatry. I feel privileged to follow Ted Stern's long and successful tenure and look forward to building upon the strong foundation laid out by earlier chief editors, Wilfred Dorfman and Thomas Wise."
Psychiatry Postdocs Highlighted at National Postdoc Appreciation Week
Friday, September 18, 2020
National Postdoc Appreciation Week (NPAW) is coming up next week, and we are proud to share that two of our Psychiatry postdocs are selectees in this year's NPAW Postdoc Showcase! Michelle Carr, PhD and Erinn Duprey, PhD will present their research on Lucid Therapy Dreaming Effects on Sleep, Mood, and Well-Being and Child Maltreatment and Youth Suicide: Implications for Prevention, respectively. Be sure to vote for your top presentations for the People's Choice Award to support postdoc great research!
RSVP at bit.ly/URNPAW2020 to check out the presentations, as well as all the other NPAW events!
5th Annual Symposium on Behavioral Health Integration Goes Virtual!
Wednesday, September 9, 2020
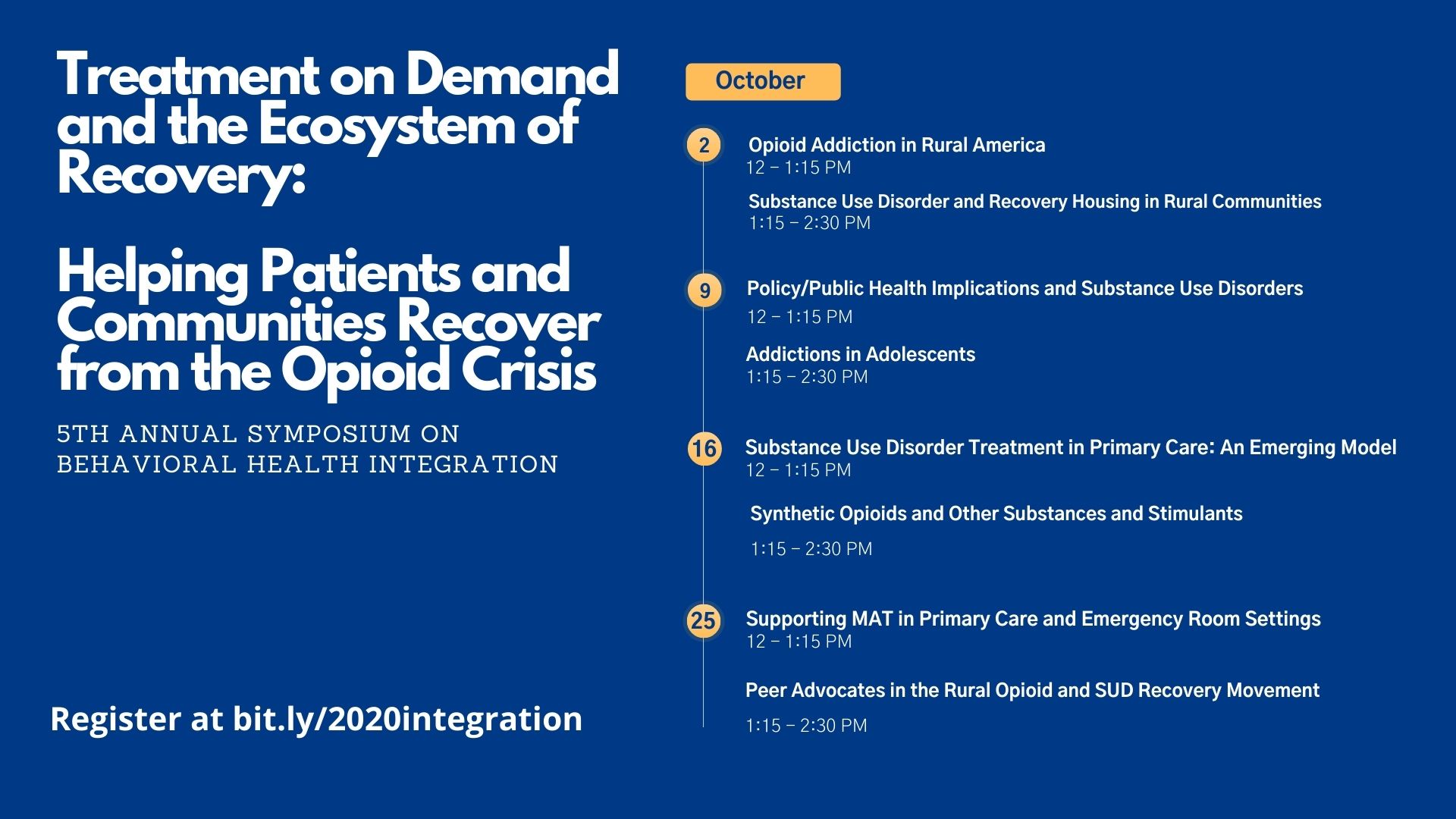
The Department of Psychiatry Collaborative Care and Wellness Division will be hosting the 5th Annual Symposium on Behavioral Health Integration virtually throughout the month of October! This year's symposium, Treatment on Demand and the Ecosystem of Recovery: Helping Patients and Communities Recover from the Opioid Crisis, will feature experts every week discussing challenges and strategies for addressing the opioid epidemic, with a focus on rural communities.
July Psychiatry Publications
Wednesday, September 9, 2020
- Mark Oldham, MD and Hochang Ben Lee, MD were coauthors on a paper discussing cognitive, psychiatric, and quality of life outcomes in adult survivors of Extracorporeal Membrane Oxygenation Therapy.
- Steve Silverstein, PhD led a study on differences in retinal structure in individuals with schizophrenia and their implications in understanding broader aspects of pathophysiology, neurodevelopment, and neurodegeneration.
- Steven Lamberti, MD and Robert Weisman, DO wrote an article on forensic assertive community treatment (FACT) and meeting the needs of justice-involved individuals with serious mental illness.
- Julie Lutz, PhD and Kimberly van Orden, PhD published a paper in Medical Clinics of North America on differentiating psychiatric illness versus normative developmental sadness and worry in older adults.
- Elizabeth Karras, PhD was a coauthor on this study in The American Journal of Health Promotion looking at correlates of refusal to firearm-related survey items.
- Ian Rockett, PhD was a coauthor on a paper on the feasibility of a standardized dual screening for suicide and overdose.
Faculty Members Join Expanded Roles
Monday, August 17, 2020
We are excited to share that a number of faculty members have been named to new expanded roles within UR Medicine.
Linda Chaudron, MD will serve as director of a newly formed URMC Center for Gender and Leadership upon her return from a year-long partial sabbatical to develop plans for a new faculty and staff leadership development function while becoming director of the Paul M. Schyve, M.D. Center for Bioethics. As director of The Center for Gender and Leadership, Chaudron will lead efforts to develop leadership skills in faculty and staff across URMC. READ MORE>>
Michael Hasselberg, PhD, has been appointed as UR Medicine's first senior director of Digital Health. In this role, Hasselberg will be in charge of developing the strategy for implementing digital health solutions throughout UR Medicine. READ MORE>>>
Kenya Malcolm, PhD has been named Director of Infant and Early Childhood Initiatives for the Division of Child and Adolescent Psychiatry. Malcolm currently leads a grant project for training and implementation of Healthy Steps in Pediatric Primary Care Practice in Golisano Children's Hospital. She also serves as the lead supervisor for clinical care for patients 0-5 years old seen in our Pediatric Behavioral Health and Wellness Service.
Andrew Cohen, PhD has been named Director of Behavioral Health and Collaborative Care for Pediatric Practice. In this role, Cohen will be working with large, diverse, multidisciplinary teams in Golisano Children's Hospital's Pediatric Primary Care Practice to promote care integration and best meet the behavioral health and psychosocial needs of patients and families.
Kathleen Baynes Named Recipient of Faculty Training Initiative
Monday, August 10, 2020
Congratulations to Kathleen Baynes, MD on being selected as the 2020 recipient for the American Academy of Child and Adolescent Psychiatry's (AACAP) Psychodynamic Faculty Training and Mentorship Initiative! As part of this initiative, Baynes will work with national leaders in youth psychodynamic psychotherapy education as she implements a project focused on improving faculty skills as supervisors here at University of Rochester. Results of this project will be presented at the next annual meeting of the AACAP.
Speaking on Bayne's accomplishments, Michael Scharf, MD says "Those of us who work closely with Kathleen already know what an outstanding clinician and educator she is how lucky we are to have her as a faculty member and Director of our Child and Adolescent Psychiatry Fellowship -- and I'm sure we can all agree it is wonderful to see her recognized nationally as well!"
New Adult Outpatient Mental Health Services Building Officially Opens
Wednesday, August 5, 2020
In July, our new Adult Outpatient Mental Health Services building officially opened at 150 North Chestnut Street. We look forward to continuing to serve the Rochester community through our new expanded location. Our new facility is conveniently located between the Central Business District and South Marketview Heights and provides a warm, inclusive atmosphere for our current and future clients. This new location will be the largest adult mental health clinic in downtown Rochester and consolidates services previously offered at our Strong Hospital and Science Parkway locations in one convenient building in the heart of Rochester. Lazos Fuertes, which is also moving to N. Chestnut Street, is the only all bi-lingual and bi-cultural mental health clinic of its kind in the county. A recording of the event can be viewed online.
The grand opening of our new Adult Outpatient Mental Health Services building was also featured on 13WHAM ABC,News 8 WROC, and Spectrum News.
Psychiatry Awarded Additional $2.5M to Combat Opioids in Rural Communities
Monday, July 20, 2020
URMC's Department of Psychiatry has been awarded an additional $2.5 million to expand the scope of its UR Medicine Recovery Center of Excellence project, bringing total funding from the Health Resources and Services Administration (HRSA) to $9.17 million.
The project focuses on assisting rural communities, particularly in Appalachia, with implementing evidence-based practices that reduce the use of and overdose from synthetic opioids. The additional funding will allow for the development and sharing of materials in four areas:
- Reducing stigma, self-stigma and shame
- Addressing and preventing opioid-related suicide
- Improving methadone accessibility in rural opioid treatment programs
- Providing accessible treatment to patients released from correctional facilities
The center, one of three Rural Centers of Excellence on Substance Use Disorder in the country, provides organizations across the U.S. with the practical tools they need to support program development. These tools have been adapted specifically for rural communities, which face a unique set of challenges in addressing this crisis. The center also provides coaching and technical assistance as organizations work through planning and implementation challenges.
The dissemination program grant from HRSA retains its original three-year timetable and service area of 23 counties in New York, Ohio, Kentucky and West Virginia.
"Over the first six months of our work, we confirmed that many Appalachian communities and collaboratives have established successful evidence-based programs that are positively impacting this crisis,said Michele Lawrence, MBA, MPH, assistant vice president of Regional Business Development for URMC and co-principal investigator for the project." We look forward to highlighting many of those in our webinars over the next two years. However, other communities are still not sure where to begin or how to build on their initial success. This generous increase in funding allows us to expand our breadth of programming and the depth of our technical assistance into areas where we know they are struggling."
"One area we have heard about from organizations across the U.S. is stigma,"said addiction medicine expert Gloria J. Baciewicz, MD., professor of Clinical Psychiatry, senior medical director of URMC's Strong Recovery program, and co-principal investigator for the project. "There continues to be a range of values and beliefs embedded in the fabric of our communities that prevent us from fully recognizing persons with substance use disorders among us and engaging the community, families, employers, providers and patients in creating an environment that supports recovery and ultimately improves the overall economic resilience and health of our communities. Together, we can have a more significant, sustainable impact as we work to defeat the opioid crisis that is ravaging our society."
The center also has seen additional needs emerge as a result of the current pandemic. Treatment programs have had to redesign operations, and the UR Medicine Recovery Center of Excellence has shared its struggles and successes with those challenges. Patients who may have been in recovery for months or years face new difficulties as the social support system they rely on has drastically been altered. The center is pushing out information in July to help patients and providers across the U.S. access life-saving drugs such as naloxone by mail and maintain that social support through new types of communities, all of which can be found on the website.
"Our team has partnered in a unique way with rural Appalachian communities, researchers, clinicians, community based organizations and more," said Psychiatry Hochang B. Lee, M.D., and John Romano, Professor of Psychiatry. "They are reducing the impact of synthetic opioids by recognizing the power of each of us to contribute to the health of our community."
Michael Hasselberg Appointed URMC Senior Director of Digital Health
Monday, July 20, 2020
To capture the vast opportunity that emerging technologies present in reshaping the future of health care, URMC appointed Michael Hasselberg, M.S., Ph.D., associate professor of Psychiatry and Clinical Nursing, to serve as its first senior director of Digital Health.
Hasselberg, an ANCC Board-Certified Psychiatric Nurse Practitioner with a PhD in Health Practice Research from the University of Rochester School of Nursing, assumed his role July 1, and reports directly to URMFG CEO Michael F. Rotondo, M.D.
As senior director, Hasselberg will be charged with developing the strategy for implementing digital health solutions throughout UR Medicine. By optimizing existing programs and accelerating new technologies, Hasselberg will seek to differentiate UR Medicine to our patients, expand our market and offer high-value care delivery in support of our "think digital first" philosophy.
"We had identified Mike as our digital health leader due to his solid track record of successfully launching innovative digital solutions with Project ECHO and his position as Co-Director of the Health Lab," Rotondo said. "But like many things these past few months, we put a pause on finalizing his role due to COVID. Not surprisingly, Mike's talents shone during the pandemic, as he led a team to develop and launch Dr. Chat Bot for URMC, the highly successful COVID-19 screening tool being used at URMC, the University—and now available to all organizations nationally."
"This role is even more critical now as we adapt our clinical enterprise to new models of care we'll need to safely interact with our patients to provide care and treatment," Rotondo added.
"Michael brings unique expertise to an area of need for our institution," said Gregg T. Nicandri, MD, FAOA, Chief Medical Information Officer and Associate Professor of Orthopaedic Surgery. "During the COVID-19 pandemic, we have been working closely on many projects including telemedicine, patient and employee screening, surge planning, and operational reporting. We have made significant strides in our enterprise digital health capabilities. During a very challenging time for our clinical operations, Michael has demonstrated highly effective leadership. I look forward to working with him, and am excited for what URMC's future holds."
Hasselberg founded the UR Medicine Telepsychiatry program and has served as an expert advisor on digital health to the New York State Department of Health, the Department of Health & Human Services, the American Hospital Association, and the National Quality Forum. A Robert Wood Johnson Foundation Clinical Scholar Fellow, he also serves as the Chief Innovation & Technology Officer in the Department of Psychiatry. He will maintain these responsibilities at varying levels of time and workload.
"In my new role, I hope to make URMC a national leader in using digital technologies the way tech industry giants like Amazon and Google do—by deeply understanding who their customers are, anticipating their needs and preferences, and delivering services that are high-quality, cost-efficient and responsive," Hasselberg said. "COVID really fast-tracked us into what the future of health care is going to look like—it's going to be a digital world. There is no going back."
Hasselberg will collaborate with colleagues at the University and across the medical system, including the chief medical and nursing technology officers, to integrate emerging technologies into the electronic health record platform in a way that synchs up and improves day-to-day operations.
But that's just a start. Hasselberg points to a host of other promising avenues to explore to improve health care outcomes, as well as the experience for patients and health care providers alike. These technologies include machine learning analytics in EHRs to risk-stratify patients and predict who will do better with various care pathways; collecting and using data from patients' wearable devices like Apple Watches and Fitbits and integrating that data into the EHR; touchless technology and speech recognition that will go far beyond mere scribing for providers; mobile apps for android and IOS devices plus web-based applications; augmented reality and virtual reality. 
"These may seem futuristic, but many are already in use and demonstrating value here," Hasselberg said. "We have brilliant folks at the University of Rochester in computer engineering and data science, and a world-renowned optics program. PROMIS is a huge patient-reported outcomes data repository—the largest in the world. We have assets that no one else has, and we can be national leaders in this field."
8th Annual Summer Series Discusses Anti-Racism & Transformation
Monday, July 6, 2020
Our 8th Annual Summer Series, held in partnership with the Department of Neurology and Department of Pediatrics, will begin on July 8th, and presentations will continue on the 2nd and 4th Wednesdays of July and August. To capitalize on the current strides being made in the growing recognition of systemic, structural racism as our number one public health threat, this year's series is designed to help University employees broaden their understanding of themselves in relation to racism with a focus on how to become an anti-racist activist. Through didactics and small group conversations, personal, programmatic, and institutional actions will be jump started throughout the summer months.
In addition to these biweekly presentations, small group intensives will be held on the 1st and 3rd of July and August with exercises provided at the presentations the week prior. Space is limited for groups.
As PRIDE month comes to a close...
Monday, July 6, 2020
As June is ending and we approach July, the month Rochester has historically celebrated Pride, we want to make sure that our department takes a moment to reflect on the needs of the communities we serve, the legalized discrimination that impacts so many, and our own biases. All too often, our education system does not teach us about the historical experiences of diverse communities.
Anti-Mask and masquerade laws originated in the 1800's in response to individuals wearing disguises to evade taxes or debt. Over time, these laws were applied to lesbian, gay, bisexual transgender, queer, and questioning (LGBTQ+) communities. Specifically, the "three-piece law" which required individuals to wear at least three articles of clothing socially connected to their sex assigned at birth was used. While this was never an actual law, police routinely pulled individuals into restrooms or less private spaces to visually "verify" their sex matched their clothes. More recently, this law was used in response to Occupy Wall Street.
These Anti-mask laws were a catalyst for LGBTQ+ Rights Movement. On June 28, 1969, police raided the Stonewall Inn, but this time the patrons refused to go to the bathroom with police to be violated and degraded through anti-mask laws. After the police were especially physical with some of the women, an uprising occurred, and many individuals credit transgender women of color for being the first to stand up to the police that night. The following year the first Pride march occurred in NYC, and here we are 50 years later. Amidst pandemic and Black Lives Matter movement, many Pride festivals across the country have transformed into marches for both Black Lives Matter as well as Pride or were cancelled altogether (i.e., due to COVID).
With each step forward, there is often a step backwards. This year the Supreme Court has voted in favor of protecting LGBTQ+ individuals from employment discrimination just after President Trump pushed forward with healthcare rollbacks that can significantly affect the basic healthcare of transgender and gender diverse individuals. In addition, one of Rochester's gems, the Out Alliance, has recently closed its doors, taking with it a vital safe space, advocacy, and education center for the Rochester LGBTQA+ community.
Therefore, as clinicians, researchers, scholars, administrators, and staff, please take a moment to acknowledge or listen to the experiences your co-workers, patients, and participants often go through on a daily basis. Question what you are doing to learn about Black history, LGBTQ+ history, and the barriers that so many face, especially Black transgender individuals. While URMC has again been acknowledged by the HRC as a LGBTQ Healthcare Equality leader, so much work is needed. Feel free to reach out to our Office of DICE, Megan Lytle, or local resources for more information on what you can do. There are Allyship Workbooks, guidelines, and information available to start this process.
Multi-Year Grant to Study Peer-Led Vaping Prevention Program in Middle Schools
Wednesday, June 24, 2020
A new $4 million, five-year grant will enable researchers at the University of Rochester Medical Center to study the effectiveness of peer-led efforts to prevent adolescent vaping in schools.
The project, funded by the National Institute on Drug Abuse (NIDA), will center on a program called "Above the Influence of Vaping" (ATI-V). Started in 2017, ATI-V engages eighth graders to create a school culture in which more students overcome pressures to abuse vaping. Key opinion leaders selected from diverse friendship groups go through training to learn what motivates them to rise above negative influences, in particular what they gain in life by not vaping, versus what they lose if they do. They also learn how peer norms drive behaviors and their role in shifting attitudes toward vaping resistance. After training, peer leaders lead prevention campaigns with adult mentors in their school and disseminate ATI-V to their friends. The prevention campaigns use science-validated strategies, which peer leaders adapt for their local school culture.
"Eighth grade is a fairly early stage of experimentation with vaping products, which makes that age an optimal window to engage key opinion leaders before attitudes normalizing vaping become widespread," said Peter Wyman, Ph.D., professor of Psychiatry, lead investigator, and director of the School and Community-Based Prevention Program at URMC. "School districts are extremely receptive to students taking the lead and working with adults in the school to strengthen resistance around vaping use."
Wyman and his colleagues saw early evidence of ATI-V's effectiveness during a pilot project conducted during the 2018-19 school year. Working with eighth-grade peer networks in three schools, ATI-V identified and trained 50 peer leaders to disseminate vaping-prevention messages among friends. Twelve to 16 weeks afterward, students with more of these peer leader friends were less likely to report vaping.
ATI-V is based on a social network approach. Many new behaviors spread through peer friendship networks, with key opinion leaders playing an influential role by introducing new practices and encouraging others to adopt them. Research shows vaping prevention is well-suited to this approach because peer group attitudes are influential in adolescents' decisions to try vaping products.
This new project will work with eighth and ninth graders at 20 schools across the Finger Lakes Region and Western New York, including a mix of urban and rural locations. The study will test if ATI-V reduces vaping behaviors by 10th grade by increasing students' perceptions that vaping is unacceptable to peers and has social costs. The program will also examine if ATI-V bolsters connections to positive adults who support non-use decisions, and increases social influence of non-using students.
The project will also look to identify implementation barriers by comparing three schools that successfully implemented ATI-V with three that struggled to adopt it, in order to identify what implementation strategies would be needed above and beyond the current ATI-V. New York State agencies including Mental Health, Addiction Services and Supports, and Education will assist in disseminating what is learned through the project.
The comprehensive school-wide approach used by ATI-V is needed due to the increase of vaping among teen and young adult populations, and the demand from school communities to see more interventions that can be tailored to local needs, according to Wyman.
"Two years ago, vaping was taking off due to several factors, including new products that delivered high doses of nicotine. We were hearing from adults in the schools that there was a tremendous need to start prevention, as well as from older teens who wished they had resisted vaping before becoming dependent. And since there was no evidence base of research-informed programs, we adapted our peer-led Above the Influence -- which started as an overall substance abuse program -- and focused it on vaping prevention."
Research shows that adolescent vaping has been spreading rapidly. The proportion of 10th- and 12th- grade students reporting regular nicotine vaping (16.1% and 21%, respectively) in 2018 was double the rate from 2017. Since 2018, rates of vaping have continued to rise. Evidence also exists that early nicotine exposure can act as a gateway to using other substances and may increase risk for addiction.
In order to identify peer leaders, this project will work with each school to send out an initial, anonymous survey of eighth graders to identify social groups and influential opinion leaders.
"We focus on opinion leadership for a fairly small group. For the eight or nine students that hang out together, one or two of those students are usually influencers. ATI-V aims to activate those influencers with the intent of long-lasting impact to prevent initiation of vaping within these peer friendship groups," Wyman said.
May 2020 Publications
Tuesday, June 23, 2020
- Several members of Psychiatry published a paper in Psychiatric Services assessing the impact of the Inpatient Medicine in Psychiatry Unit on important hospital process metrics. Authors included Marsha Wittink, MD, Wendi Cross, Phd, Jacqueline Goodman, MA, Heather Jackson, RN, MS, Telva Olivares, MD, Hochang Ben Lee, MD, Dukjae Maeng, PhD, and Eric Caine, MD.
- An article by Mark Oldham, MD was published in Psychosomatics discussing how personalities can inform clinical care.
- Joshua Wortzel, MD led a paper on recent trends in mental health clinical research in PLOS ONE. Christopher Fragassi, MD, Virginia Ramos, MD, and Hochang Ben Lee, MD also contributed to this article.
- Wilfred Pigeon, PhD, Todd Bishop, PhD, and Liz Karras, PhD were co-authors on a paper in Frontiers in Psychiatry exploring the use of administrative data to predict suicide in the veterans health system.
- Members of the HOPE Lab, published a paper on ways to help our older patients stay socially connected during physical distancing, including making a Connections Plan.
- Jaclyn Kearns published in General Hospital Psychiatry a review on sleep and suicide risk in youth. Wilfred Pigeon, PhD also was a coauthor on this paper.
- Steve Silverstein, PhD led a study in Biomarkers in Neuropsychiatry on the connection between retinal changes and neurodegenerative disorders.
- Yeates Conwell, MD led a study published in American Journal of Geriatric Psychiatry on peer companionship's mediating relationship with depression and anxiety in older adults. Kimberly van Orden, PhD and Carol Podgorski, PhD were co-authors on this paper.
- Khushminder Chahal MD, Mark Oldham, MD, and Mark Nickels, MD published a study on preferred kinds of communication in consultation-liaison services in Psychosomatics.
Virtual Graduation Ceremony Celebrates Residency and Fellowship Graduates
Tuesday, June 9, 2020
We are again forced to change an honored tradition in our department as a result of the ongoing COVID-19 crisis. For the first time in 74 years, our department will not have a Key Day Ceremony and will instead, we will be combining elements of the Key Day Ceremony with our various disciplines' graduation dinners or ceremonies.
A Virtual Graduation Ceremony was held to celebrate our residency and fellowship graduates took place on Wednesday, June 10th. Short speeches honoring graduates were given by program directors and awards were given out.

Congratulations to the following:
Psychiatry Graduates
- Andrew Martina
- Lorangelly Rivera
- Samantha Kamp
- Kelly Lamb
- Mustafa Rehmani
- Larry Sorrell
- Mark Messih
- Maura Tappen
- Brittany Mott
- Jessica Ee
- Tom Jacob
- Emily Clark
- Adrianna Hitchins
Psychology Graduates
- Aileen Aldalur
- Rachael Arowolo
- Jia Hui "Yvonne" Chaw
- Melissa Dudley
- Shiloh Eastin
- Sarah Georgianna
- Jeremy "Mac" Kelly
- Elisabeth "Lizzie" O'Rourke
- Marisa Malone, Ph.D.
- Lindsay Sycz, Psy.D.
To read more about our grads, visit our 2020 Celebration Headquarters website! Congratulations again to all our grads, and we look forward to seeing your next steps!
Practical Tips for Family Wellness during COVID-19 Webinar Scheduled for May 29th
Wednesday, May 27, 2020
Please join a panel of Psychiatry experts on May 29th at 12:00pm for a free virtual town hall focused on practical parenting tips, strategies for family resilience and more.
Speakers include:
- Ben Lee, MD, Chair, Department of Psychiatry
- Melissa Heatly, Ph.D., Clinical Psychologist, School Mental Health Initiatives
- Aparajita 'Tuma' Kuriyan, Ph.D. -- Clinical Psychologist, Family Engagement Specialist
- Kenya Malcolm, Ph.D. --Clinical Psychologist, Early Childhood Mental Health
- Linda Alpert-Gillis, Ph.D. -Clinical Psychologist, Director, Pediatric Behavioral Health & Wellness
- Jim Wallace, MD., Psychiatrist, Child & Adolescent Psychiatry, Project TEACH
- Tony Pisani, Ph.D., Clinical Psychologist, Center for the Study and Prevention of Suicide
Kelly Vandermark Featured in UR Medicine Primary Care
Wednesday, May 13, 2020
Kelly Vandermark is building a bridge.
After more than a decade working as a Strong Recovery addiction specialist, she's forging a connection with Primary Care aimed at bringing services to people where they are, when they need them.
"It's a different way of approaching substance use disorder and treatment—going to the patient when they're in a crisis so we can catch them during that vulnerable time and link them to treatment," Vandermark says. Her newly created position straddles Strong Recovery and Primary Care in an effort to create a long-term sustainable approach to identifying and treating substance use disorder (SUD).
As a credentialed alcoholism and substance abuse counselor (CASAC), Vandermark has close to 25 years of experience in addiction therapy. She also holds a master's degree in health administration.
Now she is Primary Care's go-to for helping patients with substance use disorders who may need treatment, including medication-assisted therapy (MAT). "I'm here to link them to the help they need," Vandermark says.
She's also leading the way in creating a deployable CASAC unit, "So we can travel throughout the Primary Care network, bringing services to our patients. We will meet them in their doctor's office, assess their needs, and collaborate with their provider to come up with a treatment recommendation so everyone can work as a team," she says.
This connection aims to improve Primary Care patients' access to Strong Recovery's expanded stabilization program, which provides immediate treatment for patients as young as age 14 and can get them started on medication-assisted therapy with buprenorphine. Once stabilized, they are referred back to their primary care provider to continue their treatment, with Vandermark's support as needed.
"There's a misconception that people have to wait to get into treatment, but there is actually access to care the same day—which is key," Vandermark says. "This program offers a great opportunity to access that care and to raise awareness among providers of all the resources we have to help them care for their patients."
And given the network's geographic size, Vandermark is also interested in reaching out to offices beyond Monroe County to understand the resources they have and learn how they can work together to meet their communities' needs. "This is where we really want to develop mobile services, which may include things like telemedicine and providing treatment in rural primary care offices, to address barriers to treatment," she says.
Vandermark is uniquely qualified to launch this new position. With her long-term experience in the field, she brings a wealth of knowledge of all the resources available in Monroe County and beyond.
"It's a really exciting opportunity. I'm not aware of anything else like it on an outpatient basis," she says. "This is just the beginning. We're very much in the developmental stages and I'm excited to play a role in getting it up and running.
"I'm also excited and grateful to have this opportunity to work with Rob Fortuna, Alisa Stetzer and their team in developing best practices for opioid prescribing," Vandermark adds. "This team has welcomed me as a resource in working with the two opioid care managers, Terri Dale and Barb Myers. They assist providers and patients in tapering off of opioids safely and their groundwork has paved the way for my added resources."
 "I've only been working with Kelly for the last few months, though in that short time I have come to appreciate her breadth and wealth of information in substance use disorders—assessments and treatment, etc.," says Alisa Stetzer, director of Care Management for Primary Care. "I learn so much each time I meet with her. She is very team-oriented, warm and creative, with a 'can-do' attitude. I've been having a fun time collaborating with her, and look forward to more!"
"I've only been working with Kelly for the last few months, though in that short time I have come to appreciate her breadth and wealth of information in substance use disorders—assessments and treatment, etc.," says Alisa Stetzer, director of Care Management for Primary Care. "I learn so much each time I meet with her. She is very team-oriented, warm and creative, with a 'can-do' attitude. I've been having a fun time collaborating with her, and look forward to more!"
Vandermark keeps busy on the home front, too. With John, her husband of 25 years, free time is often filled with their kids' sporting events. Patrick, 21, is an aspiring PA studying biology and playing football at St. Lawrence University; Brianna, 19, played travel soccer and is in nursing school at LeMoyne College; and Tyler, 17, plays football for Webster Thomas High School.
The Vandermarks have achieved a level of fame around their Webster neighborhood—thanks to their "celebrity dogs"—two Newfoundlands. At 125 pounds and 150 pounds, you can't miss them!
Psychology Day is May 27th!
Thursday, May 7, 2020
Mark your calendars -- Psychology Day is May 27th this year!
 Thank you to all of our fabulous psychologists and psychology trainees for ALL that you do, in so many places! Our department has many faculty psychologists who provide clinical services and research initiatives across the medical center and throughout our community. We are so proud of our American Psychological Association accredited Doctoral Internship (Adult and Child/Adolescent tracks) and Postdoctoral Fellowship (Integrated Care Family and Child/Adolescent tracks) programs which prepare outstanding clinical psychologists for careers in patient care, teaching, scientific research, and administration. We appreciate you all every day, not just on Psychology Day!
Thank you to all of our fabulous psychologists and psychology trainees for ALL that you do, in so many places! Our department has many faculty psychologists who provide clinical services and research initiatives across the medical center and throughout our community. We are so proud of our American Psychological Association accredited Doctoral Internship (Adult and Child/Adolescent tracks) and Postdoctoral Fellowship (Integrated Care Family and Child/Adolescent tracks) programs which prepare outstanding clinical psychologists for careers in patient care, teaching, scientific research, and administration. We appreciate you all every day, not just on Psychology Day!
For the first time, the annual Psychology Day at the U.N. will be a virtual event. Celebrate with us and the U.N.!
On social media? Share in the international celebrations via hashtags: #PsychologyDay2020 and #PsychDayUN2020. Thanks for all that you do!
A Person-Centered, Integrated Team Approach for Patients With Severe Mental Illnesses
Wednesday, May 6, 2020
Several members of Psychiatry recently published this paper in Psychiatric Services exploring the impact of a specialized medical unit using a biopsychosocial model to care for patients with severe mental illnesses. The study assessed the impact of the Inpatient Medicine in Psychiatry Unit on important hospital process metrics, notably reducing length of stay and improving discharge to home and readmission rates. Authors included Marsha Wittink, M.D., Wendi Cross, Ph.D., Jacqueline Goodman, MA, Heather Jackson, R.N., M.S., Telva Olivares, M.D., Hochang Ben Lee, M.D., Dukjae Maeng, Ph.D., and Eric Caine, MD.
Psychiatry Residents Selected for American Psychiatric Association Fellowships
Thursday, April 23, 2020
Three residents in our Psychiatry Residency Program were recently selected for fellowships with the American Psychiatric Association (APA).
- Carla Velarde, M.D., was selected for an APA SAMHSA Funded Minority Fellowship Program. This program provides a one-year minimum fellowship to psychiatry residents who are committed to becoming a leader in the field of minority psychiatric mental health issues.
- Emilie Transue, M.D., was selected for an APA Public Psychiatry Fellowship Program. This program provides support for a group of outstanding residents interested in the field of public and community psychiatry.
- Joshua Wortzel, M.D. was selected for an APA Leadership Fellowship Program. This program provides psychiatry trainees opportunities to interact with national thought leaders in the field and to further develop their professional leadership skills, networks and psychiatric experiences.
Congratulations to our residents for these well-deserved opportunities!
Suicide Prevention During the Pandemic: An International Panel Conversation
Wednesday, April 22, 2020
Supporting suicide prevention in our communities is more important than ever as we contend with the international Covid-19 pandemic. In a panel, hosted by American Foundation for Suicide Prevention chief medical officer Christine Moutier, M.D. and University of Rochester prevention expert Anthony R. Pisani, Ph.D., experts from four continents will share their experiences and perspectives. The webinar will take place on April 27th, 2020, starting at 4 PM.
Panelists include
- Yeates Conwell, M.D., University of Rochester, United States. Older adult suicide prevention, extensive experience in China.
- Carrie Lumby, Illawarra Shoalhaven Suicide Prevention Collaborative, Australia. Suicide prevention community advocate / lived experience expertise.
- Maurizio Pompili, Ph.D, Sapienza University of Rome, Italy. European suicide prevention, psychiatry education, Italian experience with COVID.
- Paul Yip, Ph.D., DCS, University of Hong Kong, HKSAR. Suicide and SARS epidemic, youth suicide prevention and crisis intervention.
April 2020 Publications
Thursday, April 16, 2020
-
Catherine Glenn, Ph.D. led a study published in the Journal of Child & Adolescent Psychology on the feasibility and acceptability of intensive ecological momentary assessment among high-risk adolescents with suicidal thoughts and behaviors following discharge from acute psychiatric care.Yeates Conwell, M.D. and Linda Alpert-Gillis, Ph.D. were also co-authors on this paper.
-
Steven Lamberti, M.D., Viki Katsetos, M.D., David Jacobowitz, M.A., and Robert Weisman, D.O. recently published an article looking at the relationship between psychosis, mania and criminal recidivism in Harvard Review of Psychiatry.
-
Mark Oldham, M.D., led a study published in the Journal of Psychosomatic Medicine on integrating proactive, multidisciplinary mental health teams and provider and nursing satisfaction. Patrick Walsh, Ph.D., Daniel Maeng, Ph.D., and Hochang Ben Lee, M.D. were co-authors on this paper.
-
Lisham Ashrafioun, Ph.D., Todd Bishop, Ph.D., Peter Britton, Ph.D., Wilfred Pigeon, Ph.D., and Cathleen Kane of Canandaigua VA Medical Center published a study looking at the link between reported pain intensity and suicide attempts in veterans.
-
Daniel Maeng, Ph.D., Jennifer Richman, M.D., Hochang Ben Lee, M.D., and Michael Hasselberg, Ph.D. published in the Journal of Psychosomatic Medicine a paper on the impact of integrating psychiatric assessment officers via telepsychiatry on rural hospitals' emergency revisit rates.
-
Lauren DeCaporale-Ryan, PhD, Jessica Goodman, PhD, Adam Simning, MD, PhD, Lara Press-Ellingham, MPA, Linda Williams, BSN, RN, and Michael Hasselberg, PhD published in the American Journal of Geriatric Psychiatry a study looking at staff training and Process Group Intervention as a method of addressing psychosocial needs in nursing homes during the COVID-19 pandemic.
Department of Psychiatry Grand Rounds Halted for 2020
Thursday, March 19, 2020
Our Department of Psychiatry Grand Rounds have been temporarily halted for the safety and well being of our faculty, staff, and students. In its place, the Psychiatry Department is holding a series of COVID-related Cyber Town Hall Meetings Wednesdays at Noon, via Zoom. For more information regarding what the department is doing to help in this difficult time, please see our Coronavirus Info page.
Psychiatry Joins Annual NAMIWalks For 2020
Friday, March 6, 2020
The Department of Psychiatry will once again be joining the annual NAMIWalks Rochester on May 2nd, 2020! Four teams from Psychiatry will be walking- Psychiatry Ambulatory Nurses/Techs, Department of Psychiatry Advisory Council of Consumers (DPACC), 3-9000, and Psychiatric Emergency- to support NAMI Rochester's services.
Interested in supporting NAMI Rochester and the free advocacy, support and education they provide to clients and families? Join the walk or donate! You can also contribute to our teams' donation goals by searching for the team name on the NAMIWalks Rochester website.
Todd M. Bishop Receives Sleep Grant Award During National Sleep Awareness Month
Wednesday, February 26, 2020
The Hypersomnia Foundation recently awarded a grant to Todd M Bishop, Ph.D. Not only is Dr. Bishop an Assistant Professor within the Department of Psychiatry, he also holds appointments as a researcher and Assistant Director of Fellowship Training at the VA Center of Excellence for Suicide Prevention.
Dr. Bishop's awarded work will center on the development and validation of a case ascertainment algorithm for idiopathic hypersomnia within the electronic medical record of the Veterans Health Administration. Subsequently, the study team will aim to 1) estimate the prevalence of IH diagnosis among the Veteran population, 2) facilitate an examination of treatment utilization patterns and prescribing practices, and 3) explore co-occurring physical and behavioral health conditions with an emphasis on suicide risk factors. He has been invited to present details of this sponsored work at the Hypersomnia Foundation's Annual Conference in June.
People Born Blind Are Mysteriously Protected From Schizophrenia
Monday, February 17, 2020
Steven Silverstein, Ph.D. recently spoke with VICE on the complex relationship between congenital blindness and schizophrenia.
"I was struck by how many of the compensations that the brain seems to make, or the skills that blind people develop, seem to be the exact opposite of what you find in schizophrenia," he says.
January 2020 Publications
Monday, February 10, 2020
- The Journal of Interprofessional Care featured a study by Marsha Wittink, MD and co-authors Jennifer Funderburk, PhD, and Wilfred Pigeon, PhD exploring team-based approaches to suicide prevention.
- Jack Peltz, PhD published in Sleep a study looking at parent-set bedtimes, sleep deprivation, and depressive symptoms in teens. Peltz completed this study as part of a research appointment in the Department of Psychiatry.
Linda Chaudron Featured in "Women, Unlimited" Article
Friday, January 31, 2020
Linda Chaudron, MD, Associate Vice President and Senior Associate Dean for Inclusion and Culture Development at URMC, was featured in the "Women, Unlimited" cover story of the latest issue of Rochester Medicine. "Women, Unlimited" highlights accomplishments of trailblazers and new leaders that are driving the advancement of women in medicine. In this interview, Dr. Chaudron discussed closing the gender gap in health care.
New Chief Social Worker
Thursday, January 30, 2020
Jewell Hopkins is a Rochester native and Chief Social Worker for the Department of Psychiatry SMH Social Work. She completed graduate school at Stony Brook University with the intent of obtaining a dual degree in Law and Social work. However, after starting her social work courses she had an instant connection with the field and realized it “fit with who she was.”
Much of Jewell’s passion and background revolves around children’s behavioral health. She loves working with kids, specifically on a micro level. Her first position out of graduate school was as Crisis Specialist with the Youth Emergency Services Program at Crestwood (a part of Hillside Children’s Center). Jewell spent quite a bit of time working at Hillside, where she further developed skills in day treatment, outpatient, crisis stabilization and in-home preventive programs. For Jewell, it was “good to see people in their own environment, to see beyond their challenges and see their growth.” Jewell also served as a Juvenile Justice Clinical Coordinator, a collaboration with Monroe County Office of Mental Health, Probation, and the Department of Human Services, assisting family court judges and probation officers with identifying and assessing youth with potential mental health issues and linking families to services.
Jewell began her career at UR Medicine as an inpatient medical social worker providing support on a medical/surgical unit where she gained a wealth of knowledge about the adult medicine world and a deep appreciation for the vast ways in which social workers can function and be effective in this field. She moved on to become the senior social worker for a Transitional Housing Project, which helped to identify and assist with problem solving around housing needs for patients at URMC.
Jewell loves the many different facets of the social work profession and the ways in which it allows a person to be “part of someone’s journey of healing and wholeness.” While social workers can take on many different roles and scopes within the department and across UR Medicine, what Jewell feels they hold consistent is the value and goal of serving those in need. She added that, "transitioning to psychiatry has been a learning process that has provided many opportunities to collaborate and grow, and the best part has been getting to know many wonderful people in psychiatry and across every discipline." She believes social work brings “support, advocacy, and empowerment to our department, not only for the patients but for our colleagues as well.”
Jewell emphasizes teamwork, saying: “We must work as a team so we are able to make a difference and promote the vision of providing good quality care.” For Jewell, the change and difference we are making are for the benefit of the community and she hopes that we can continue to reflect that approach. She adds: “I value and appreciate the hard work and dedication of every social worker and it has been a pleasure learning and seeing the impact of our profession across the department!”
In addition to the joy she gets from her career, Jewell enjoys and appreciates the art of music, which stems from playing the piano and cello as a child and through high school. She hopes that in the future she can reignite her passion of cello playing.
Future Behavioral Health Center Aims to Ease Demand for Adolescent, Children's Services
Wednesday, January 29, 2020
13 WHAM ABC recently discussed our Golisano Pediatric Behavioral Health and Wellness Building under construction off South Avenue.
Speaking on the new facility as well as the need for "right-sized programs" for youth, Michael Scharf, M.D., says, "Kids who are at a crisis level of severity, who'd potentially be in an inpatient unit, can come in and get the same level of intensity of treatment that you could get in the hospital."
Jeff Lyness Awarded 2020 APA Vestermark Psychiatry Educator Award
Wednesday, January 29, 2020
Jeff Lyness, MD has been selected as the recipient for the 2020 Vestermark Psychiatry Educator Award. This annual award is given by the American Psychiatric Association (APA) and recognizes an psychiatric educator for outstanding contributions to psychiatric education. As part of this award Lyness will present the annual Vestermark lecture at the 2021 APA Annual Meeting.
Two Honored With Presidential Diversity Awards
Tuesday, January 28, 2020
Kit Miller, director of the MK Gandhi Institute for Nonviolence, and Caroline Nestro '18W (PhD), a senior associate in the Department of Psychiatry, are the recipients of the 2020 Presidential Diversity Award.
The honor is presented annually to recognize faculty, staff, students, units, departments, or teams that "demonstrate a commitment to diversity and inclusion through recruitment and retention efforts, teaching, research, multicultural programming, cultural competency, community outreach activities, or other initiatives."
URMC Awarded $6.7M to Combat Opioid Crisis in Rural Communities
Wednesday, January 15, 2020
The Department of Psychiatry of the University of Rochester Medical Center has been named one of the three Rural Centers of Excellence on Substance Use Disorder in the country, and awarded a $6.7 million federal grant to identify and adapt evidence-based practices that effectively impact synthetic opioid morbidity and mortality in rural Appalachian communities.
The three-year dissemination program grant, from the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services, will connect leaders in substance use disorder and rural medicine from the UR Medicine Recovery Center of Excellence with local community leaders and health care providers across 23 counties in New York, Ohio, Kentucky and West Virginia.
$3.6M NIH Grant Funds Center for Social Ties and Aging Research
Friday, January 10, 2020
Caring for a family member with dementia creates both challenges and opportunities for families. Strong social connections can help caregivers manage the challenges, but the demands of caregiving sometimes create obstacles to social connections. When this happens, caregivers may experience social isolation and loneliness, adding to stress, low quality of life, and increased risk for poor health.
A new center at the University of Rochester is bringing together researchers to find new and innovative ways to promote social connectedness and the overall health of older adults caring for a loved one with dementia.
The Roybal Center for Social Ties and Aging Research (STAR), a joint initiative between the UR School of Nursing and the Department of Psychiatry, is funded by a $3.6 million grant from the National Institutes of Health. The center will focus on fostering collaboration among researchers to make a significant impact on the problem of social disconnection in older caregivers of individuals with Alzheimer's Disease and other related dementias (ADRD). Its major activity will be funding pilot studies through its annual Pilot Award Program. Requests for proposals will be announced in the next several months.
Adolescent, Young Adult Clinics Open at UR Medicine’s Strong Recovery, Strong Ties
Tuesday, January 7, 2020
Unique programs offer integrated substance use disorder and mental health treatment services
UR Medicine Mental Health and Wellness has opened two new Community Division programs that provide comprehensive care for adolescents and young adults facing both substance use and mental health concerns:
Strong Recovery's Adolescent and Young Adult Program is the region's only Certified Community Behavioral Health Clinic (CCBHC) to provide comprehensive treatment for adolescents and young adults who are struggling with substance use and co-occurring mental health disorders, such as depression and anxiety.
Strong Recovery is an exclusive clinic consisting of an Adolescent Program for patients ages 14- to 18-years-old, and an Emerging Young Adult Program for those age 18 to 24. It offers an environment tailored to the specific needs of this population related to addiction, while also providing support to patients' families, significant others, legal guardians, mentors and friends to help patients maintain recovery and find a successful path to wellness.
Strong Ties Young Adult Program, also a Certified Community Behavioral Health Clinic (CCBHC), offers specialized early intervention treatment for young adults 18- to 28-years-old, struggling with serious mental health concerns such as schizophrenia, with or without substance use issues. The Young Adult Program is a subspecialized clinical pathway, part of the larger Strong Ties Clinic that has received national recognition for providing comprehensive mental health treatment for individuals across the adult age continuum for decades.
TRANSFORM Center To Hold Meet and Greet
Monday, January 6, 2020
Join Sheree Toth, Executive Director of Mt. Hope Family Center, Jody Todd Manly, Clinical Director of Mt. Hope Family Center, Catherine Cerulli, Director of Laboratory of Interpersonal Violence & Victimization, and special guest Adam Bello, Monroe County Executive Elect, in the TRANSFORM Research Center's inaugural Meet and Greet event on January 7th, 2020 at Knoblauch Gallery. The purpose of this event is to introduce the TRANSFORM Research Center and to connect organizations across disciplines working with children and child maltreatment.
TRANSFORM (Translational Research that Adapts New Science FOR Maltreatment) is a national resource center that conducts research, disseminates discoveries, and builds on state-of-the-art research and practices to foster the next generation of interdisciplinary professionals committed to preventing and addressing child abuse and neglect. Partners include the Susan B. Anthony Center, Mt. Hope Family Center, Laboratory of Interpersonal Violence and Victimization, as well as the University of Minnesota Education Development Center and Institute for Translational Research on Children's Mental Health.
