CHeT Outcomes
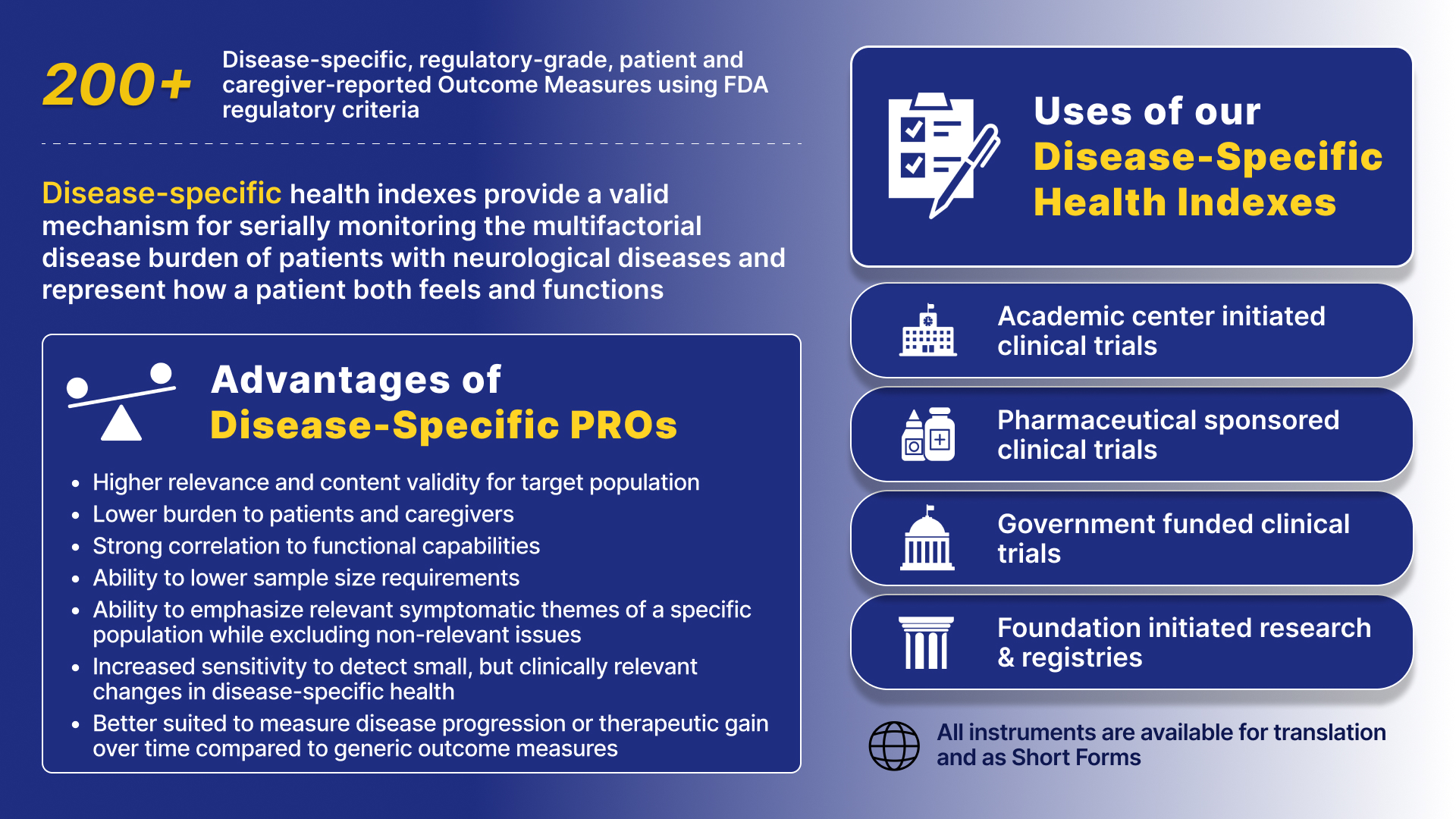
The CHeT Outcomes team specializes in developing and validating highly sensitive, disease-specific outcome measures, reported by patients (PRO: patient-reported outcomes) and caregivers (CR: caregiver-reported outcomes, also known as ObsRO: observer-reported outcomes). These measures are designed for use in therapeutic trials and FDA drug-labeling claims. Our group has developed and individually validated more than 200 disease-specific instruments and over 1000 subscales that quantify symptomatic disease burden during clinical trials. These instruments are capable of reliably measuring how a patient feels and functions, can reduce sample size requirements, and are designed to detect meaningful changes in health prior to traditional and generic outcome measures.
Our disease-specific instruments have demonstrated superior responsiveness in detecting clinically relevant changes in patient conditions compared to traditional measures. View our 5 Pivotal Studies to learn more about these findings.
Our Instruments
Our instruments measure the multifaceted, patient-perceived disease burden in individual diseases. Our team of epidemiologists, biostatisticians, qualitative researchers, patient advocates, linguists, computer programmers, outcomes researchers, and physicians has developed patient-reported and caregiver-reported outcome measures for adult and pediatric populations, including instruments for the following diseases:
- Adrenoleukodystrophy (ALD)
- Adrenomyeloneuropathy (AMN)
- Alzheimer's disease (CI)
- Amyotrophic lateral sclerosis (ALS)
- Cardiomyopathy
- Cerebral cavernous malformation (CCM)
- Charcot Marie Tooth (CMT)
- Crohn’s disease (CD)
- Dementia (CI)
- Duchenne muscular dystrophy (DMD)
- Dystonia
- Facioscapulohumeral muscular dystrophy (FSHD)
- Fibromyalgia (FM)
- Fragile X
- Friedreich’s ataxia (FA)
- Huntington’s disease (HD)
- *Integral in obtaining FDA drug approval
- Inclusion body myositis (IBM)
- Limb Girdle Muscular Dystrophy (LGMD)
- Lung cancer (LC)
- Lysosomal acid lipase deficiency (LAL-D)
- Mild cognitive impairment (CI)
- Mitochondrial disease
- Myasthenia gravis (MG)
- Myotonic dystrophy type 1 (DM, DM1, MDHI)
- *NIH gold standard for therapeutic trials
- Myotonic dystrophy type 2 (DM2, MD2HI)
- Non dystrophic myotonia (NDM)
- Parkinson’s disease (PD)
- Rheumatoid Arthritis
- SCN2A
- SHANK3 / Phelan McDermid Syndrome
- Smith Magenis Syndrome / RAI1
- Spinocerebellar ataxia (SCA)
- Spinal-bulbar muscular atrophy (SBMA)
- Spinal muscular atrophy (SMA)
- SYNGAP1
- “Human-HI”: Human Health Index
Our group will collaborate with you to develop and fully validate a disease-specific outcome measure for any disease or provide consultation regarding outcome measure selection, use, optimization, and analysis. If you would like more information about how you can obtain a license to use our health indexes in your study, please contact HealthIndexes@chet.rochester.edu