News
New Studies Suggest Vaping Could Cloud Your Thoughts
Monday, December 28, 2020
Two new studies from the University of Rochester Medical Center (URMC) have uncovered an association between vaping and mental fog. Both adults and kids who vape were more likely to report difficulty concentrating, remembering, or making decisions than their non-vaping, non-smoking peers. It also appeared that kids were more likely to experience mental fog if they started vaping before the age of 14.
While other studies have found an association between vaping and mental impairment in animals, the URMC team is the first to draw this connection in people. Led by Dongmei Li, Ph.D., associate professor in the Clinical and Translational Science Institute at URMC, the team mined data from two major national surveys.
"Our studies add to growing evidence that vaping should not be considered a safe alternative to tobacco smoking," said study author Li.
The studies, published in the journals Tobacco Induced Diseases and Plos One, analyzed over 18,000 middle and high school student responses to the National Youth Tobacco Survey and more than 886,000 responses to the Behavioral Risk Factor Surveillance System phone survey from U.S. adults. Both surveys ask similar questions about smoking and vaping habits as well as issues with mental function.
Both studies show that people who smoke and vape -- regardless of age -- were most likely to report struggling with mental function. Behind that group, people who only vape or only smoke reported mental fog at similar rates, which were significantly higher than those reported by people who don't smoke or vape.
The youth study also found that students who reported starting to vape early -- between eight and 13 years of age -- were more likely to report difficulty concentrating, remembering, or making decisions than those who started vaping at 14 or older.
"With the recent rise in teen vaping, this is very concerning and suggests that we need to intervene even earlier," said Li. "Prevention programs that start in middle or high school might actually be too late."
Adolescence is a critical period for brain development, especially for higher-order mental function, which means tweens and teens may be more susceptible to nicotine-induced brain changes. While e-cigarettes lack many of the dangerous compounds found in tobacco cigarettes, they deliver the same amount - or possibly more - nicotine.
While the URMC studies clearly show an association between vaping and mental function, it's not clear which causes which. It is possible that nicotine exposure through vaping causes difficulty with mental function. But it is equally possible that people who report mental fog are simply more likely to smoke or vape -- possibly to self-medicate.
Li and her team say that further studies that follow kids and adults over time are needed to parse the cause and effect of vaping and mental fog.
In addition to Li, authors of the youth study include Catherine Xie, and Zidian Xie, Ph.D. For the adult study, Li was joined by co-authors Zidian Xie, Ph.D., Deborah J. Ossip, Ph.D. Irfan Rahman, Ph.D., and Richard J. O'Connor, Ph.D. Both studies were funded by the National Cancer Institute and the U.S. Food and Drug Administration's Center for Tobacco Products.
Researchers Draw More Links between Vaping, Smoking, Young People, and Coronavirus
Wednesday, September 9, 2020
What do vapers, smokers, and non-smokers with chronic conditions such as high blood pressure or diabetes have in common? They all are at higher risk for COVID-19.
The scientific explanation behind this is complex and not yet certain — but it may boil down to an enzyme known as ACE2, that lives on the surface of many cells in the lungs and serves as the entry point for the coronavirus.
Evidence shows that people with chronic inflammatory illnesses, vulnerable older adults, and those who smoke or vape, all have an abundance of ACE2 receptor proteins to serve as a gateway to the deadly virus.
A research team at the University of Rochester Medical Center, led by Irfan Rahman, Ph.D., published a series of studies during the pandemic that focus on the vital role of ACE2 — which is already at the center of many other scientific investigations — to shape a clearer picture of the critical cellular mechanisms that regulate the deadly virus and its link to vaping.
While Rochester investigators are working in lockstep with scientists around the world, Rahman's special interest is on the growing problem of young people who test positive and may be spreading coronavirus at alarming rates. Even some older children and teens who have higher levels of the ACE2 receptor seem to be more vulnerable to the virus.
"Our next step is to investigate whether ACE2 is normally low in young people, hence their relatively low infection and mortality rates from COVID-19, but to find out if ACE2 is increased by smoking or vaping rendering them more susceptible to the virus," said Rahman, Dean's Professor of Environmental Medicine, Medicine (Pulmonary), and Public Health Sciences. "This would be in contrast to older people with lung diseases such as COPD and pulmonary fibrosis, who we already know are at higher risk for severe viral illnesses and death."
Coordinating Coronavirus Research: Creating Options for Our Sickest COVID-19 Patients
Tuesday, July 14, 2020
When the first COVID-19 cases hit the University of Rochester Medical Center's ICU back in March of 2020, there were no proven treatments available, but experimental therapies were cropping up around the world. Quickly, a team of URMC clinicians and researchers mobilized to bring the most promising clinical trials - that address the broadest swath of patients' needs - to URMC. Since then, URMC has joined three clinical trials that provide extra treatment options for some of the sickest COVID-19 patients.
COVID-19 causes a wide range of outcomes: some infected people never show a single symptom, while many battle the disease for weeks in the ICU. The difference between those outcomes seems to lie in a careful balance of the immune response. In the beginning of the disease, the immune system helps fight off the virus. But for those who land in the hospital, this early, helpful immune response gives way to uncontrolled over-activation of the immune system, causing system-wide inflammation and severe complications.
The three COVID-19 inpatient clinical trials currently running at URMC attack the disease at both ends of this balance.
"Our goal has always been to promote effective therapies through clinical trials," said Martin Zand, M.D., Ph.D., senior associate dean for Clinical Research and co-director of the Clinical & Translational Science Institute. "Our team is working hard to make sure that the trials we bring to URMC have the greatest chance of benefiting our own patients, and significantly advancing the science of COVID-19 to benefit patients around the world."
Quieting Inflammation at All Ages
While researchers have high hopes that baricitinib can quell the over-exuberant immune activity of COVID-19, that trial is only open to patients who are 18 years old and up. Another trial, sponsored by Incyte Corp, is testing a very similar drug, called ruxolitinib, in patients as young as 12 who have very severe COVID-19 disease and need to be on a ventilator.
When the immune system runs amok in the late stages of COVID-19, the lining of the lungs can become leaky, allowing fluid to build up in the lungs' air sacs. This phenomenon, called acute respiratory distress syndrome, starves the body of oxygen and mechanical ventilation can even fail to rescue these patients.
The URMC team, led by Christopher Palma, M.D. and Steve Georas, M.D., expects to enroll up to 20 severely ill COVID-19 patients in the trial to see if ruxolitinib can keep them alive and get them off ventilators and out of the ICU sooner.
URMC research uncovers links between COVID-19 and vaping, smoking
Monday, June 29, 2020
Research at the University of Rochester Medical Center has found evidence of why COVID-19 is worse for people who smoke and vape than for the rest of the population.
Irfan Rahman, who runs a lab at URMC that studies the effects of tobacco products on the lungs, said people who smoke and vape often have elevated levels of receptors for an enzyme called ACE2.
Those receptors also allow the novel coronavirus to enter lung cells. More receptors means more viral load, which means more severe infections, Rahman said.
"It's pretty bad, actually," he said.
Rahman said early evidence from novel coronavirus infections showed that smokers were particularly at risk from COVID-19, but the mechanism behind the vulnerability was unclear.
Now, Rahman and other researchers said, a growing body of evidence shows inhaling nicotine increases the lungs' receptiveness to the virus and the lethality of the disease.
Other articles on this topic:
Rahman Lab Highlighted in Nature
Thursday, June 11, 2020
The Rahman lab has been highlighted in Nature journal for their work on discovery of exosomes in COPD. Read the article.
Tom Mariani Receives Andy Tager Award for Excellence in Mentoring
Wednesday, May 27, 2020
Please congratulate Tom Mariani, who is this year's recipient of the Andy Tager Award for Excellence in Mentoring!
Tom's dedication to scientific inquiry into lung biology, and his enduring effort to lift all boats with a rising tide made him the perfect fit for this award!
"Assembly on Respiratory Cell & Molecular Biology Andy Tager Award for Excellence in Mentoring"
Dr. Andy Tager was a remarkable physician scientist who combined his talent as an astute and caring physician, with that of a creative and insightful scientist, and with a lifelong dedication to helping others. Dr. Tager received multiple national awards for his discovery of bioactive lipids as potential targets of therapy in interstitial pulmonary fibrosis and distinguishing himself as one of the few to fulfill the dream of taking his work from bench to bedside. He was a selfless mentor to trainees and colleagues at his home institution, caring for the careers of those he was mentoring at least as much as his own. Less obvious to others, through his many leadership roles at ATS, Dr. Tager helped promote the professional careers ATS of members, particularly the RCMB Assembly, from all over the world. The Andy Tager Award for Excellence in Mentoring is our tribute to the brilliant, caring man, whose selfless dedication touched so many hearts, in more ways than one."
Matthew D. McGraw, 2020 Furth Fund Awardee
Thursday, May 7, 2020
Matthew D. McGraw, M.D., Assistant Professor, Pediatric Pulmonology and EHSC member, School of Medicine and Dentistry. McGraw recognized the need for additional research in the field of developmental biology and pulmonary toxicology. His research goal is to become a sustained contributor to in vitro and animal modeling of childhood fibrotic airways disease. These efforts will ultimately advance the health of children with debilitating lung diseases. McGraw's motivation, creativity, and intelligence will help propel his research work at the Medical Center.
Congratulations Matt!
Georas, Mariani & Dean Awarded Grants
Monday, April 27, 2020
Congratulations to Lung Biology Program members Drs. Georas, Mariani and Dean who all received the following grants:
P.I.: Steve Georas, MD
NIH/NIAA
Award Number : 1 R01 AI144241-01A1
Title of Project: Novel role of protein kinase D in airway inflammation and antiviral immunity
Project Period: 3/13/20 -- 2/28/25?
P.I.: Tom Mariani, PhD
Agency: CTSI Pilot Project Program/NIH
Award Period: 7/1/20 -- 1/31/21
Total Award (TPC): $50,000
Title: Airway Biomarkers for Prediction of ARI Etiology (Internal Grant)
The overall goal of this project is to show that airway sampling will provide optimal diagnostic biomarkers for determining bacterial involvement in ARI.
P.I.: David Dean ,PhD
Agency: NIH/NHLBI
Award Period: 4/5/20- 3/31/24
Total Award (TPC): $2,298,764
Title: A multimodal delivery and treatment approach for Acute Lung Injury (R01)
This projects investigates how gene transfer of the b1 subunit of the Na,K-ATPase to the lung increases not only alveolar fluid clearance, but also improves alveolar-capillary barrier function by up regulating abundance and activity of tight and adherent junction complexes.
P.I.: David Dean, PhD
Agency: NIH/NIDDK
Award Period: 4/15/20 -- 3/31/23
Total Award (TPC): $1,588,524
Title: Gene therapy for GERD-associated esophageal epithelial barrier dysfunction (R01)
Gen transfer of the b1 subunit of the Na,K-ATPase can upregulate tight and adherence junctions abundance and activity in the lung. Since a hallmark of gastroeosphageal reflux disease (GERD) is reduced barrier function in the distal esophagus (which may play a role in ultimate transition to esophageal adenocarcinoma), this project investigates whether gene delivery of the b1 subunit of the Na,K-ATPase can restore esophageal barrier integrity and therefore reduce GERD.
P.I.: David Dean, PhD
Agency: Cystic Fibrosis Foundation
Award Period: 2-1-20 -- 1-31-23
Total Award (TPC): $840,000
Title: : Electroporation-mediated gene delivery to the airways to treat Cystic Fibrosis (grant)
This project investigates whether electroporation-mediated gene transfer can be used to effectively sustain long-term expression of CFTR in animal models. If successful, the project may lead to the development of new therapies designed to treat people with cystic fibrosis.
As Vaping-Related Illnesses Rise, Researchers Search for Answers
Wednesday, January 15, 2020
Electronic cigarettes have been around for over a decade, but that's a relatively short time in the world of science and medicine. So very little is known about the long term health effects, like what the flavors and propellants may be doing to the respiratory system.
But as research picks up on that, what's even more pressing right now, is understanding the vaping products people are getting on the streets that is making them sick and even causing deaths.
Pulmonary scientist Irfan Rahman has been studying the impact of electronic cigarettes on the lungs. We followed him to a vape shop in Rochester, NY. He often visits many of the stores surrounding his lab at the University of Rochester Medical Center.
Rahman's team has found and published research that shows the combination of nicotine, flavors and propellants in e-juices changes cells in the lungs. "Anything [that] goes in the lung, it has to be pure. It has to be fresh," said Rahman, "[the] lung is not meant for these chemicals."
There is a growing body of research like this, showing that while vaping may be less harmful to the body than smoking, it's not exactly safe because it may affect the lungs' ability to protect against foreign agents.
Dr. Ronald Crystal, chairman of Genetics at Weill Cornell Medicine did a small study with non-smokers, who have never vaped, and gave them electronic cigarettes with a very small amount of nicotine.
"There were biologic changes. And what's clear is that if you vape, then you are going to change the biology of the cells lining your airways. Of course, the important question is, does that lead to this disease?" said Crystal. "Nicotine itself probably changes the biology of the airway cells. But probably more concerning are the contaminants and that is the flavoring that goes into [the vaping liquid], the propellants that go into it."
Researchers at URMC applaud federal vape ban, hope for further restrictions
Friday, January 3, 2020
As the federal Food and Drug Administration announced an impending ban on certain types of e-cigarettes, researchers at the University of Rochester applauded the move, but they also said it should only be the start of more regulations.
"It's a great decision," said Irfan Rahman, who runs a lab at URMC that studies the liquids used in e-cigarettes to figure out exactly what they contain.
"It should be a gateway to banning other products," he continued.
The ban will cover only certain types of e-cigarettes. Starting next month, companies will not be allowed to sell flavored vaping cartridges that contain nicotine -- with exceptions for tobacco and menthol flavors.
The rules also carve out an exception for larger "open-tank" e-cigarettes where customers fill the reservoirs with vaping liquid themselves.
The FDA, which funds much of Rahman's research, said the ban is targeting the vaping products most often used by teenagers and young adults. Rahman agreed, noting that the ban covers the flavors he encounters regularly in his analysis of the substances young people are vaping, such as bubble gum, candy or mango. "There are so many of them," he said.
"They look like they are fruit juices, but they are not. They are chemicals which look they are safe, but they are not safe."
Vaping Linked to Higher Risk of Self-Reported COPD Diagnosis
Thursday, January 2, 2020
A new study reveals an elevated risk of self-reported chronic obstructive pulmonary disease (COPD) — the third leading cause of death associated with smoking — among people using e-cigarettes. People who vaped were at increased risk even if they had never smoked tobacco, which casts doubt on e-cigarette companies' claims that vaping is a safe alternative to smoking.
According to the study, people who vaped were at a 47-percent greater risk of self-reported COPD diagnosis as compared to people in the study who did not use tobacco products. Compared to ex-smokers, people who had quit smoking and switched to e-cigarettes were 27 percent more likely to report a COPD diagnosis.
The study, published by Nicotine and Tobacco Research, is based on 2016 and 2017 Behavioral Risk Factor Surveillance System (BRFSS) national survey data of nearly one million adults. Survey participants were asked whether they had ever been diagnosed with COPD by their health-care provider.
Authors of the study, which was funded in part by the University of Rochester Clinical and Translational Science Institute (UR CTSI), the National Cancer Institute and the Food and Drug Administration, are Zidian Xie, Ph.D., Deborah J Ossip, Ph.D., Irfan Rahman, Ph.D. and Dongmei Li, Ph.D.
"It is clear, based on the large sample size of this study, that there is a significant link between vaping and self-reported COPD diagnosis in adults, even among vapers who never smoked before," said lead study author Zidian Xie.
Senior study author Dongmei Li, an associate professor in the UR CTSI, added, "More long-term clinical research is needed to determine how e-cigarette use is related to COPD, but our findings are consistent with other recent studies showing that e-cigarette use is associated with respiratory issues."
"This study provides further evidence that vaping simply isn't safe," said Deborah Ossip, a tobacco research expert and professor of Public Health Sciences at the University of Rochester Medical Center. "We hope that people begin to heed this message, especially young people who think vaping is cool and who are enticed by the thousands of available flavors."
Recent statistics from the Center for Diseases Control and Prevention's National Youth Tobacco Survey demonstrated the popularity of vaping among young people in the U.S. About one of every 10 middle school students and one out of four high school students reported in 2019 that they used electronic cigarettes.
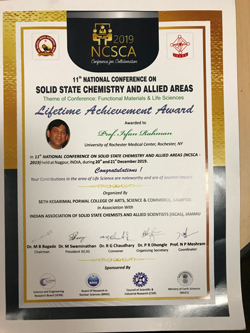
Irfan Rahman Awarded Lifetime Achievement Award at NCSCA 2019
Wednesday, January 1, 2020
Dean's Professor of Environmental Medicine, Irfan Rahman, Ph.D., was awarded the prestigious Lifetime Achievement Award by the executive committee of the NCSCA-2019 at the 11th National Conference On Solid State Chemistry And Allied Areas (NCSCA-2019), December 20, 2019. Congratulations Dr. Rahman!