Why do bones weaken in menopause, and how can that be measured?
Question: Why do bones weaken in menopause, and how can that be
measured?
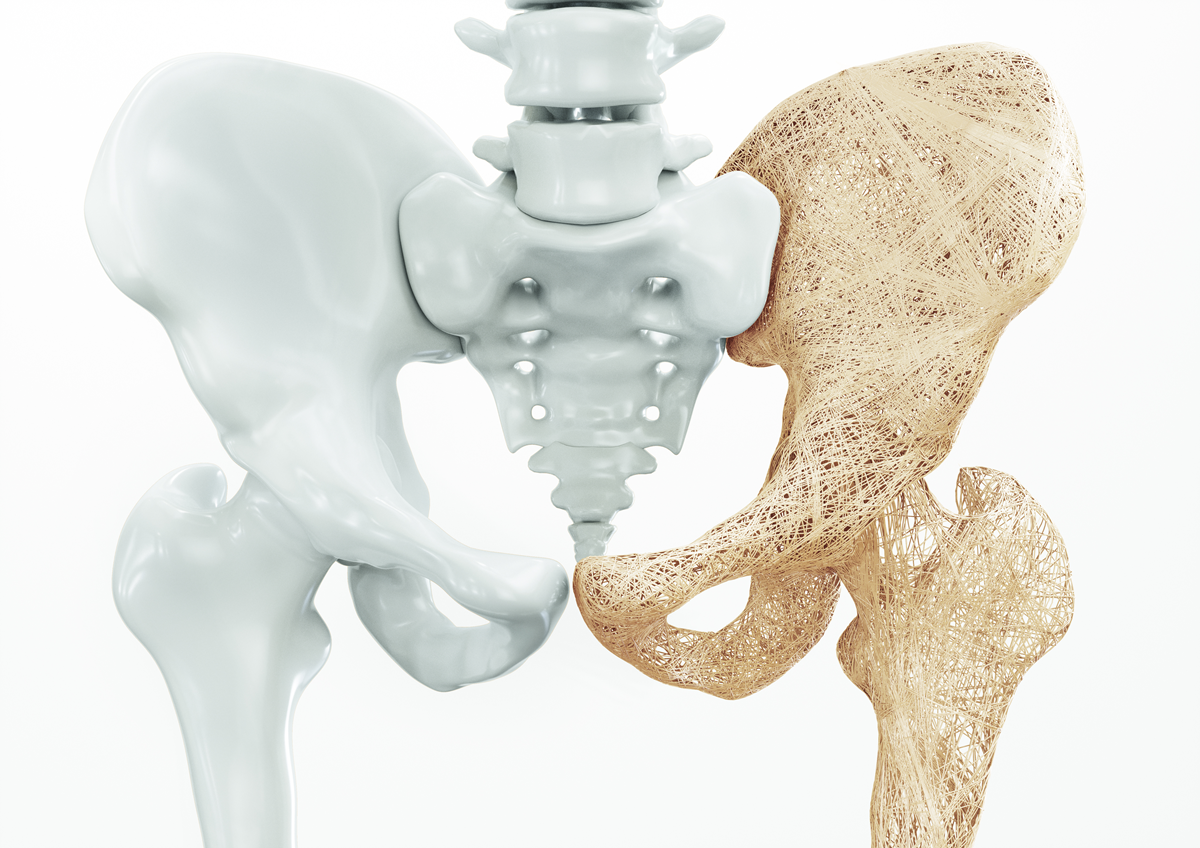
Our Response: You may be unaware that your bones are engaging in a balanced, continuous process of remodeling; laying down new bone while eliminating old bone. So why is this process jeopardized in menopause? Bone normally is produced by osteoblasts. These cells lay down a material called osteoid, composed of a collagen in a lattice frame, and fill it in with inorganic material called hydroxyapatite, which contains 99% of the body’s calcium. Bone is broken down by osteoclasts, which are derived from stem cells in the blood. Bone health is measured by bone mineral density (BMD), determined by dual-energy X‐ray absorptiometry (DXA Scan). By this technique, two X‐ray beams of different energy are aimed at bone. The results, presented as a T Score, are compared to that of the average, race‐matched, young, normal
female. Measurements of ‐1 to ‐2.5 Standard Deviations (SD) below peak normal values of the lumbar spine, or femur neck (hip), reflect low bone density (osteopenia) and ‐2.5 SD or greater reflect significant bone loss (osteoporosis). For white women over 50 years, 13% to 18% have osteoporosis of the hip, and 30% to 50% have osteopenia. By age 80, over 50% are likely to exhibit osteoporosis, making hip fractures, with a 25% mortality rate in the first year, a serious risk.
Age, a family history of osteoporosis, smoking, malnutrition, low estrogen levels, and chronic disease all are risk factors for bone loss. Because natural estradiol inhibits cytokine‐induced osteoclast activity, the expected decline of estradiol in menopause contributes to the risk of osteoporosis.
Author: James R. Woods, M.D. and Elizabeth Warner, M.D.
James Woods | 8/1/2019