Is there a higher risk for urinary tract infections (UTIs) in menopause?
Question: Is there a higher risk for urinary tract infections (UTIs) in menopause?
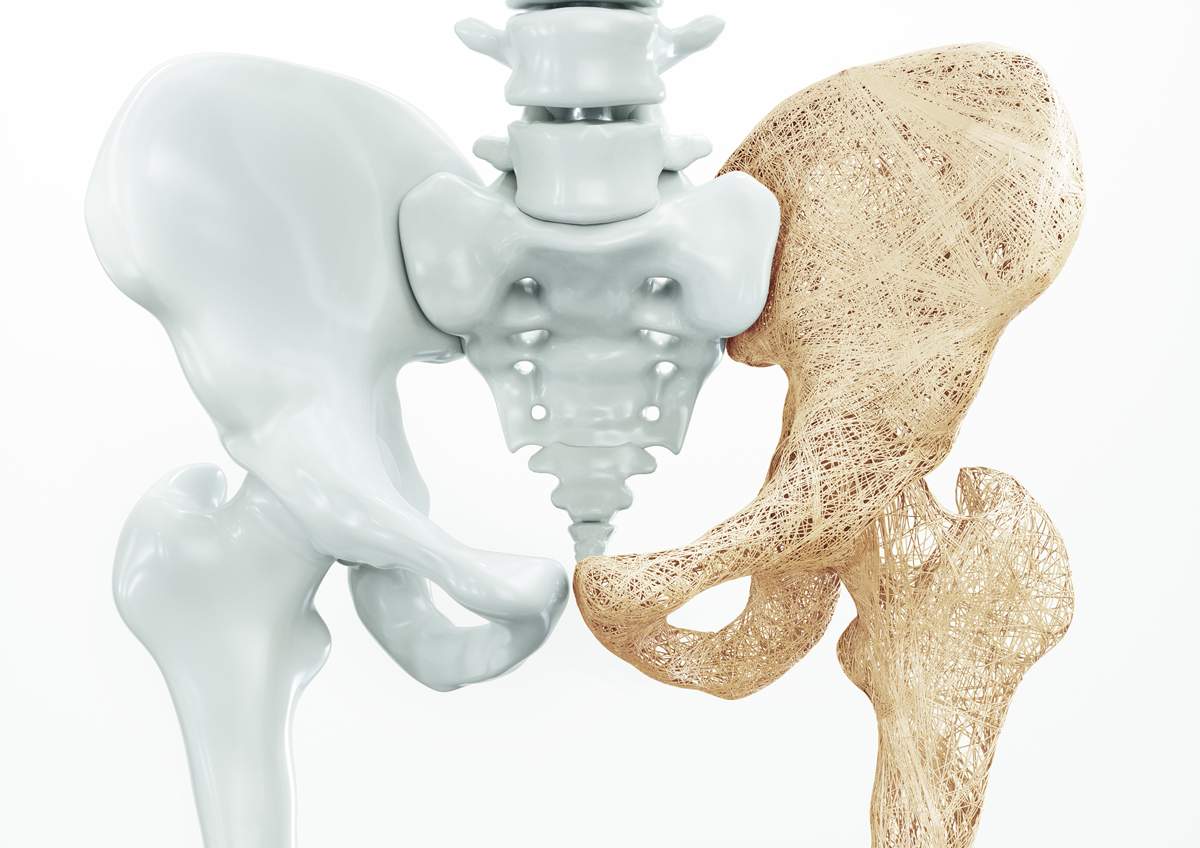
Our Response: Approximately 50% to 60% of women report at least one UTI in their lifetime. Unfortunately, the incidence of UTI increases with age and often is incorporated into the genitourinary syndrome of menopause (GSM), the leading cause of pain during intercourse. During the reproductive years, ovaries produce high levels of estradiol, which in the pelvic region acts as a powerful anti-inflammatory hormone. Estradiol also dilates pelvic blood vessels to bring in moisture, maintain a healthy acidic vaginal pH, and promote mucosal thickening. What often is overlooked, however, is that the lower bladder and urethra, by their proximity to the vagina, also benefit from the hormone changes occurring during reproductive life. During menopause, decreased estradiol eliminates the pelvic health benefits of natural hormone production. Estradiol depletion can lead to thinning and dryness of the vaginal tissues and an increase in vaginal pH. These changes are accompanied by the loss of lactobacillus, the normal vaginal bacterium, and the risk of vaginal colonization by gram-negative bacilli, the main pathogen of the urinary tract. Estrogen loss also decreases the volume of the pelvic floor musculature, allowing for the risk of pelvic organ prolapse and urinary incontinence. Both pelvic floor prolapse and urinary incontinence have been shown to increase the risk for UTIs. Unfortunately, vaginal atrophy, characterized by vaginal dryness, itching, pain on intercourse, and
urinary incontinence, can imitate a UTI when no infection is present. Vaginal estrogen reduces the incidence of UTIs and helps with vaginal symptoms that are not caused by infection. Prophylactic antibiotics can reduce the incidence of UTIs, and pelvic floor exercises help to strengthen pelvic tone.
Disclaimer: The information included on this site is for general educational purposes only. It is not intended nor implied to be a substitute for or form of patient specific medical advice and cannot be used for clinical management of specific patients. Our responses to questions submitted are based solely on information provided by the submitting institution. No information has been obtained from any actual patient, and no physician-patient relationship is intended or implied by our response. This site is for general information purposes only. Practitioners seeking guidance regarding the management of any actual patient should consult with another practitioner willing and able to provide patient specific advice. Our response should also not be relied upon for legal defense, and does not imply any agreement on our part to act in a legal defense capacity.
James Woods | 6/25/2019