Metabolic Syndrome and the Role of Estrogen

Metabolic syndrome represents a cluster of adverse biologic events characterized by alterations in lipids, elevated blood sugar, and increased cardiovascular risk. According to the National Cholesterol Education Program’s Adult Treatment Panel 111 Report, metabolic syndrome may be diagnosed when three of the following criteria are present: waist circumference greater than 88 cm, HDL-C less than 50 mg/dL, triglycerides greater than 150 mg/dL, blood pressure above 130/85 mmHg, or fasting blood sugar over 110 mg/dL. The greatest health risk of metabolic syndrome is cardiovascular disease, but this risk also is age related. Sixty percent of postmenopausal women are affected by metabolic syndrome, whereas only 22% of the general population meet these criteria. These differences in prevalence underscore the dramatic physiologic changes that occur as a woman enters menopause.
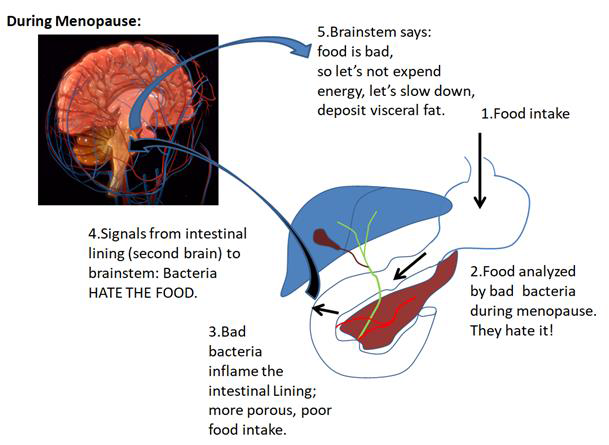
Menopause is defined as one year without menses. The menopause transition now is formally defined as the three-to-five-year period leading up to this new stage of life. This transition often is recognized by women with the onset of irregular menses and vasomotor symptoms. Often, it is characterized by increased fat depositions, especially in the intra-abdominal area (visceral fat) with little change in muscle mass. Visceral fat cells with direct access to portal blood entering the liver are a significant source of many of the inflammatory proteins felt to be responsible for cardiovascular heart disease. The appearance of these inflammatory proteins results from fluctuations and then the natural decline of ovarian estradiol, a hormone that in the pre-menopause provides anti-inflammatory protection.
Visceral obesity also correlates closely with an increase in insulin resistance leading to elevated insulin levels, abnormal glucose metabolism, and a reduction in fat breakdown. Insulin, acting through its receptors to stimulate insulin-like growth factor-2 (IGF-2), is critical for normal glucose metabolism. It transports glucose from the blood into the cells and allows fat to be broken down. Yet, insulin receptors are under hormonal control since estradiol improves insulin sensitivity and glucose metabolism while reducing body fat. Obesity, coupled with insulin resistance, results in over expression of insulin receptors, lower than normal levels of IGF-2, and production of a second growth factor, insulin-like growth factor -1 (IGF-1), which causes a pathologic process that destabilizes glucose metabolism in insulin-sensitive tissue.
Visceral fat also has a direct effect to increase appetite and reduce energy expenditure. Premenopausal estradiol maintains a balance of intestinal peptides that signal the brain when a person has eaten enough. In these women, appetite is controlled by increased adiponectin and ghrelin and decreased resistin and leptin. Yet, in obese women with metabolic syndrome and insulin resistance, adiponectin (important for cardiovascular protection) is decreased, and leptin and resistin are increased. How do we know estradiol is involved? Transdermal estradiol supplementation in these women reverses these changes. Moreover, in clinical studies, energy expenditure in obese women with metabolic syndrome is reduced but improves once transdermal estradiol supplementation is instituted.
It is not surprising that obesity, especially in the menopause transition, appears to be the primary clinical target for reducing the risk from the metabolic syndrome. Daily exercise and diet management to reduce fat, especially visceral fat, is central to this effort. Moreover, hormone supplementation with transdermal estradiol capitalizes on the effect of estradiol to increase insulin sensitivity, reduce abdominal fat, and rebalance intestinal satiety peptides.
By James Woods, M.D. and Elizabeth Warner, M.D.
Dr. Woods treats patients for menopause at the Hess/Woods Gynecology Practice.
Disclaimer: The information included on this site is for general educational purposes only. It is not intended nor implied to be a substitute for or form of patient specific medical advice and cannot be used for clinical management of specific patients. Our responses to questions submitted are based solely on information provided by the submitting institution. No information has been obtained from any actual patient, and no physician/patient relationship is intended or implied by our response. This site is for general information purposes only. Practitioners seeking guidance regarding the management of any actual patient should consult with another practitioner willing and able to provide patient specific advice. Our response should also not be relied upon for legal defense, and does not imply any agreement on our part to act in a legal defense capacity.
James Woods | 3/1/2016