Mobile Stroke Unit
Life saving stroke care in minutes.
Make Appointments & Get Care
What is the Mobile Stroke Unit?
The UR Medicine Mobile Stroke Unit is the region’s only ambulance dedicated to stroke care. Unlike a traditional ambulance, it is equipped with a CT scanner to diagnose strokes and can provide specific treatments, like clot-busting medication (tPA), before reaching the hospital.
Highly-specialized staff on the MSU include a CT scanner operator, an emergency medical technician, and a trained stroke nurse who works closely with a stroke neurologist at the hospital to choose the best treatment.
The unit is equipped with the following specialized technology:
- CT scanner
- Telehealth equipment
- Point-of-care devices to test for INR, glucose, creatinine, and other values
- Medications specific to acute stroke treatment, such as tPA (tissue plasminogen)
of 4
-

Image: Mobile Stroke Unit: The first of its kind in Update New York and the surrounding region, brings the resources of an emergency room directly to the stroke patient’s driveway.
-

Image: Interior of Mobile Stroke Unit showing the onboard CT scanner
-

Image: Interior of Mobile Stroke Unit showing the screen used for a telemedicine neurologist to join to assist in treatment.
-

Image: Interior of Mobile Stroke Unit showing a cabinet of medicines available to administer to the patient immediately.
When is the Mobile Stroke Unit dispatched?
If the initial emergency call is a suspected stroke, the Mobile Stroke Unit and a standard ambulance will be dispatched immediately to the location. If the standard ambulance arrives at the scene of the call first and determines that the individual has had a stroke, EMS staff will work with the Mobile Stroke Unit staff to provide acute stroke care.
Patients will be taken to the nearest hospital with the appropriate level of care available to treat their stroke, or to the hospital requested by the patient.
Where Is The Mobile Stroke Unit Available?
Our service area includes all of Monroe County, with plans to expand to neighboring counties over time.
-
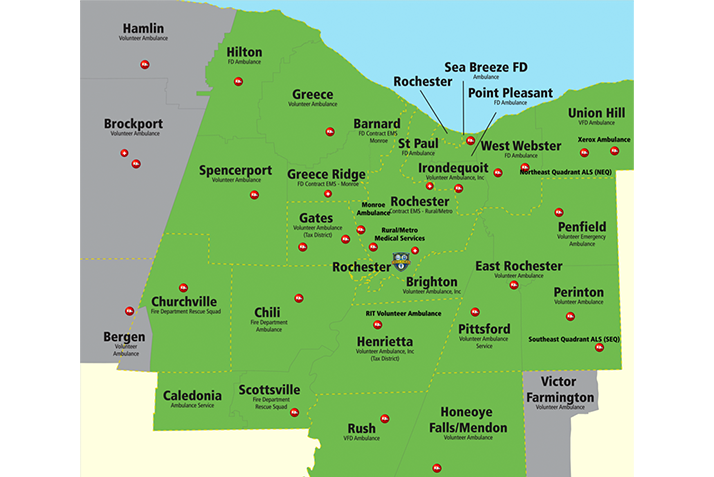
Image: A map of areas served by the Mobile Stroke Unit
UR Medicine's Approach
When someone experiences a stroke, quick, lifesaving care can greatly improve their chances of recovery and reduce disability. That’s why UR Medicine, in partnership with American Medical Response, launched our Mobile Stroke Unit.
UR Medicine has long been dedicated to providing top-level stroke care across the region, and the Mobile Stroke Unit is a key step forward in that mission.
Tarun Bhalla, MD, PhD - Director of Stroke and Cerebrovascular Services

Support the MSU
Every minute counts when someone suffers a stroke. Join us in advancing state-of-the-art stroke care by supporting this vital mobile emergency service that provides the local community their best chance at recovery.
What Sets Us Apart?
The UR Medicine MSU is the only unit of its kind in Western and Central New York and the 13th in the nation. Similar units have existed in other communities across the nation for several years. The first MSU was launched in the U.S. in Houston in 2014. Since then, MSUs have been deployed in several other cities, the closest being Cleveland and New York City. With the Mobile Stroke Unit, UR Medicine gathers data on the timeliness of stroke care and patient outcomes and uses this information to further improve stroke care.
Our nationally recognized, highly trained stroke and neurocritical care team provides comprehensive care for all types of stroke and cerebrovascular diseases. State-of-the-art neuroimaging capabilities and immediate access to all subspecialists offer patients the most sophisticated medical and surgical treatments necessary for the best outcomes.
Providers
Locations
View All LocationsWe serve you in the Rochester metropolitan area and surrounding region.
View All Locations3 locations
Clinton Crossings, Building F
2400 South Clinton Avenue
Rochester, NY 14618
Strong Memorial Hospital
601 Elmwood Avenue
Rochester, NY 14642
Highland Hospital
1000 South Avenue
Rochester, NY 14620

