News
20242023202220212020
New paper points out the need for better vision care after stroke
Wednesday, November 1, 2023
 With the global incidence of stroke on the rise and survival rates growing, there is an increase of survivors with neurological deficits related to their injury. These can include movement, speech, and, in up to 60 percent, chronic visual defects.
With the global incidence of stroke on the rise and survival rates growing, there is an increase of survivors with neurological deficits related to their injury. These can include movement, speech, and, in up to 60 percent, chronic visual defects.
Recently appointed Research Assistant Professor of Ophthalmology, Matthew Cavanaugh, Ph.D., and his collaborator Dr. Hanna Willis, at the University of Oxford, published a policy paper advocating for better screening and clinical care for patients who have suffered visual loss from a stroke. Furthermore, they go on to propose ways to accelerate research efforts to help stroke victims recover or to prevent future vision loss. Highlights from the article published in, Policy Insights from the Behavioral and Brain Sciences include recommendations to:
- Create more awareness among the clinical community and general public for the importance of immediate vision assessment of patients after stroke. Recent research suggests that early intervention during the first hours, days, and weeks after a stroke may improve visual outcomes
- Standardize care pathways for visual stroke victims so that they are treated as effectively as possible. This includes deploying machine-learning-based visual field-testing using software specifically designed to detect brain-related vision loss, versus current testing that best measures vision loss related to ocular diseases (such as glaucoma)
- Improving the network of research related to therapeutic restoration of vision, and the prevention of long-term visual degradation. A number of laboratories have developed promising therapeutic vision rehabilitation interventions to partially restore lost vision. However, none of these techniques have been deployed into medical practice
Addressing these, and other, common gaps to care and research related to visual stroke are vital. They are likely to improve the standard of care for current patients and accelerate the development of therapies to lessen the burden of this problem. Researchers like Dr. Cavanaugh, and our neuro-ophthalmology specialists at the Flaum Eye Institute are ideally positioned to help develop better solutions for this often-neglected consequence of stroke.
Huxlin, MacRae and URMC colleagues discover a new approach to treat established corneal fibrosis
Monday, October 23, 2023
 The cornea is the clear window at the front of the eye that focuses light onto the retina, enabling “vision” as we know and experience it. Infections, injury and surgery to the cornea can induce a healing response that reduces its clarity. These are leading causes of vision loss worldwide. For the last two decades, Krystel Huxlin, Ph.D., the James V. Aquavella Professor of Ophthalmology at FEI, has explored how to prevent corneal scarring after injury. Now, she and her team have discovered a novel approach to treating already established opaque corneas.
The cornea is the clear window at the front of the eye that focuses light onto the retina, enabling “vision” as we know and experience it. Infections, injury and surgery to the cornea can induce a healing response that reduces its clarity. These are leading causes of vision loss worldwide. For the last two decades, Krystel Huxlin, Ph.D., the James V. Aquavella Professor of Ophthalmology at FEI, has explored how to prevent corneal scarring after injury. Now, she and her team have discovered a novel approach to treating already established opaque corneas.
“Simply stated, healing can cause transparent corneal cells to become opaque, blocking light from reaching the retina, where it should be detected,” Huxlin said. “This transformation is defined by a series of complex events that cause corneal cells to change into myofibroblasts. As our understanding of this process has grown, we have been able to isolate key areas where we can intervene to prevent transformation. However, patients often present to the clinic after opacity and scarring have already occurred. Our lab is one of the first to ask whether it is possible to treat established fibrosis without toxic side-effects.”
A recently published paper in Investigative Ophthalmology & Visual Science, explains this concept and offers a new solution. The team performing the research included Huxlin, FEI research assistant professor Kye-Im Jeon, Ph.D., FEI cornea specialist and refractive surgeon Scott MacRae, M.D., and URMC Department of Medicine bioenergetics expert Keith Nehrke, Ph.D.
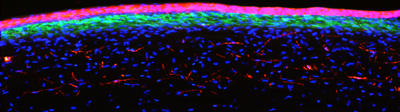 When an injury happens to the cornea, normally quiet cells called keratocytes become activated, changing into fibroblasts, and ultimately, myofibroblasts. The latter are responsible for stabilizing and repairing the wounded corneal tissue, but they are also key components of corneal scars. Many teams, including Huxlin’s, have explored ways to prevent fibrosis, which leads to scarring. This included researching methods of blocking the action of small proteins, including transforming growth factor beta, which regulate how keratocytes transform into myofibroblasts. Although these treatments can be effective, they are limited by the fact that they have to be applied immediately after injury, they cannot reverse existing fibrosis, and they can have unwanted side-effects.
When an injury happens to the cornea, normally quiet cells called keratocytes become activated, changing into fibroblasts, and ultimately, myofibroblasts. The latter are responsible for stabilizing and repairing the wounded corneal tissue, but they are also key components of corneal scars. Many teams, including Huxlin’s, have explored ways to prevent fibrosis, which leads to scarring. This included researching methods of blocking the action of small proteins, including transforming growth factor beta, which regulate how keratocytes transform into myofibroblasts. Although these treatments can be effective, they are limited by the fact that they have to be applied immediately after injury, they cannot reverse existing fibrosis, and they can have unwanted side-effects.
Huxlin and her colleagues’ new work demonstrates feasibility of a completely novel approach to the problem: manipulating a key organelle inside existing myofibroblasts, causing them to revert back to more quiescent cells. To accomplish this, the team introduced a class of compounds, called thiazolidinediones (TZD) into in vitro and in-vivo models of fibrosis. The living model involved exposing the cornea to TZDs weeks after an injury, after fibrosis had occurred. The team’s experiments showed that a particular TZD caused myofibroblasts to lose all of their defining molecular and morphological characteristics, and take on the shape and behavior of more quiescent corneal cells.
The key organelles targeted by the TZD inside myofibroblasts were mitochondria, best known for generating most of a cell’s energy and the signals used to carry out its essential functions. Thanks to the discoveries of our URMC team, mitochondria can now also be thought of as key to powering the ability of corneal myofibroblasts to remain myofibroblasts – knowledge that can be exploited to treat corneal fibrosis.
Although more needs to be understood about the effects of TZDs on myofibroblasts--such as the duration of the effect and the optimal time to apply the treatment--it represents an important step in treating corneal injuries and potentially reversing existing damage. A clinically-viable treatment would prove especially useful in regions of the world where months, even years, may pass before a patient can receive care.
Read More: Huxlin, MacRae and URMC colleagues discover a new approach to treat established corneal fibrosisFlaum Eye Institute Basic Science Seminar Series
Thursday, October 12, 2023
2023-2024 Schedule
Fridays @ 1:00pm
All seminars will be held in person
Please join via zoom if you are unable to attend in person: Zoom Link
AI helps bring clarity to LASIK patients facing cataract surgery
Wednesday, September 20, 2023
Scientists develop computer models of patients’ eyes to identify the ideal intraocular lenses and visual simulators for patients to experience how they will see with them
While millions of people have undergone LASIK eye surgery since it became commercially available in 1989, patients sometimes develop cataracts later in life and require new corrective lenses to be implanted in their eyes. With an increasing number of intraocular lens options becoming available, scientists have developed computational simulations to help patients and surgeons see the best options.
In a study in the Journal of Cataracts & Refractive Surgery, researchers from the University of Rochester created computational eye models that included the corneas of post-LASIK surgery patients and studied how standard intraocular lenses and lenses designed to increase depth of focus performed in operated eyes. Susana Marcos, the David R. Williams Director of the Center for Visual Science and the Nicholas George Professor of Optics and of Ophthalmology at Rochester, says the computational models that use anatomical information of the patient’s eye provide surgeons with important guidance on the expected optical quality post-operatively.
“Currently the only pre-operative data used to select the lens is essentially the length and curvature of the cornea,” says Marcos, a coauthor of the study. “This new technology allows us to reconstruct the eye in three dimensions, providing us the entire topography of the cornea and crystalline lens, where the intraocular lens is implanted. When you have all this three-dimensional information, you’re in a much better position to select the lens that will produce the best image at the retinal plane.”
Read More: AI helps bring clarity to LASIK patients facing cataract surgerySusana Marcos recognized at Spain’s Smart Woman Forum & Awards
Wednesday, August 9, 2023
Susana Marcos, the David R. Williams Director of the Center for Visual Science and the Nicholas George Professor of Optics and of Ophthalmology, was recognized with an award for best investigator by Spain’s Federation of Health Innovation Industry. She was recognized at the Smart Woman Forum & Awards in Madrid on July 19.
Marcos is an internationally recognized expert in the optics of the eye and the interactions of light with the retina. Her lab aims to understand the interplay of structural, biomechanical, and optical properties of the eye, their impact on retinal image quality, and the limits they impose to visual function and perception.
Susana Marcos Awarded the Edwin H. Land Medal
Thursday, April 6, 2023
 WASHINGTON – Optica (formerly OSA), Advancing Optics and Photonics Worldwide, and the Society for Imaging Science and Technology (IS&T) are pleased to announce that Susana Marcos, the David R. Williams Director of the Center for Visual Science, University of Rochester, USA, has been awarded the Edwin H. Land Medal. Marcos, a highly regarded researcher in the field of visual optics and ocular imaging, is a pioneer in the development of new techniques for the evaluation of the eye. Her work is aimed at understanding the interplay of structural, biomechanical and optical properties of the eye. Marcos studies the impact of those properties on retinal image quality, and the limits that optics impose on visual functions and perception, specifically with applications in myopia, presbyopia, cataract and corneal corrections.
WASHINGTON – Optica (formerly OSA), Advancing Optics and Photonics Worldwide, and the Society for Imaging Science and Technology (IS&T) are pleased to announce that Susana Marcos, the David R. Williams Director of the Center for Visual Science, University of Rochester, USA, has been awarded the Edwin H. Land Medal. Marcos, a highly regarded researcher in the field of visual optics and ocular imaging, is a pioneer in the development of new techniques for the evaluation of the eye. Her work is aimed at understanding the interplay of structural, biomechanical and optical properties of the eye. Marcos studies the impact of those properties on retinal image quality, and the limits that optics impose on visual functions and perception, specifically with applications in myopia, presbyopia, cataract and corneal corrections.
"On behalf of the Optica Board and membership, I am proud to congratulate Susana Marcos for this recognition," said Michal Lipson, Optica's 2023 President. "The Land Medal is awarded to individuals who share in Edwin Land's insatiable scientific intensity and curiosity in optics and imaging and, in part, reflect his image as inventor, scientist, entrepreneur, and teacher. Susana’s career journey in eye diagnostics and treatment reflects her impressive impact on the ophthalmic industry.”
Marcos joined the University of Rochester faculty in 2021 after serving as Director of the Institute of Optics, CSIC, Spain, (IO-CSIC), and Professor of Research at CSIC, where she founded the Visual Optics and Biophonics Lab (VIOBIO) in 2000. Marcos is a Fellow of Optica, the European Optical Society, and the Association for Research in Vision Ophthalmology. Marcos’ research recognitions include the Adolph Lomb Medal (Optica), ICO Prize, Doctor Honoris Causa (Ukraine Academy of Science), Ramón y Cajal Medal (Royal Academy of Sciences), King Jaime I Award, and National Research Award in Engineering.
Marcos is a cofounder of 2EyesVision SL and a coinventor of the SimVis technology that allows patients to ‘try on’ multifocal corrections before putting in contact lenses or having an intraocular lens implantation. She has authored or coauthored more than 200 peer-reviewed papers in top journals and has 23 patents (14 licensed to industry).
About the Edwin H. Land Medal
Recognizing pioneering work empowered by scientific research to create inventions, technologies, and products, the Edwin H. Land Medal was established in 1992 to honor his unique career as a scientist, technologist, industrialist, humanist and public servant. It is jointly presented by Optica and the Society for Imaging Science and Technology (IS&T) and is funded through the support of the Polaroid Foundation, the Polaroid Retirees Association and individual contributors, including Manfred Heiting, Theodore Voss and John J. McCann.
Read More: Susana Marcos Awarded the Edwin H. Land MedalPaul Dunman Elected Fellow of the American Academy of Microbiology
Tuesday, February 28, 2023
The professor of Microbiology and Immunology and Ophthalmology is one of 65 scientists selected for the 2023 fellowship class. Dunman uses Staphylococcus aureus and Acinetobacter baumannii to study how bacteria cause disease, with the goal of developing new therapies to treat bacterial infections.
Read More: Paul Dunman Elected Fellow of the American Academy of MicrobiologyGoodwill Vision Enterprises, UR Medicine Team Up to Expand Eye Care
Tuesday, January 31, 2023
Flaum Eye Institute opens new clinic in downtown Rochester
 Goodwill of the Finger Lakes and UR Medicine Flaum Eye Institute – two leaders in vision care for the Rochester region – are collaborating to improve access to best-in-class vision care in the City of Rochester.
Goodwill of the Finger Lakes and UR Medicine Flaum Eye Institute – two leaders in vision care for the Rochester region – are collaborating to improve access to best-in-class vision care in the City of Rochester.
Goodwill Vision Enterprises, formerly known as Association for the Blind and Visually Impaired, and the Flaum Eye Institute will work together to improve eye care with the expansion of low-vision care within the Sterns Center for Low Vision at 500 S. Clinton Ave., and the Feb. 13 opening of a comprehensive eye care center to serve residents of neighborhoods with limited access to this care.
“We have an obligation to ensure that we prevent blinding conditions and must do our part so all community members—including those who are uninsured—have access to routine care,” said Goodwill CEO and President Jen Lake. “This is such an important moment in time for our organization, and we are proud of our history of serving those who have low vision or are blind. This represents a new chapter for us, alongside UR Medicine Flaum Eye Institute.”
In addition to providing low-vision evaluations for individuals referred to Goodwill Vision Enterprises, Flaum will offer comprehensive eye care in the heart of downtown Rochester. There will be optometric care, screening exams for diabetes, cataracts, and glaucoma, and opportunities to obtain glasses and contact lenses.
“This is a joint effort that makes sense for both organizations. It advances our shared mission of delivering eye care to our community and working to preserve sight,” said Dr. David DiLoreto, director of the Flaum Eye Institute and chair of Ophthalmology at the University of Rochester Medical Center.
The newly renovated 5,300-square-foot suite includes six exam rooms, procedure rooms, an optical shop, and a spacious waiting area and Flaum will introduce technology upgrades, including electronic medical records, to ensure continuity of care. Four rooms will be dedicated to comprehensive eye care and two rooms will be dedicated to low-vision exams on a daily basis.
“This new site allows us to increase capacity for low-vision evaluations and minimize delays for Goodwill participants. And adding the comprehensive eye care center in the South Wedge neighborhood ensures residents have equal access to eye care,” said Dr. Christine Coward, director of the new center and chief of Flaum Eye Institute’s Comprehensive Ophthalmology & Cataract Services.
This collaborative effort allows Flaum to help reduce delays for low-vision care at the Sterns Center for Vision Care, from approximately six to two weeks and hastens referrals for low-vision rehabilitation services provided by Goodwill.
Read More: Goodwill Vision Enterprises, UR Medicine Team Up to Expand Eye Care