News
Imaging the secret lives of immune cells in the eye
Friday, October 9, 2020
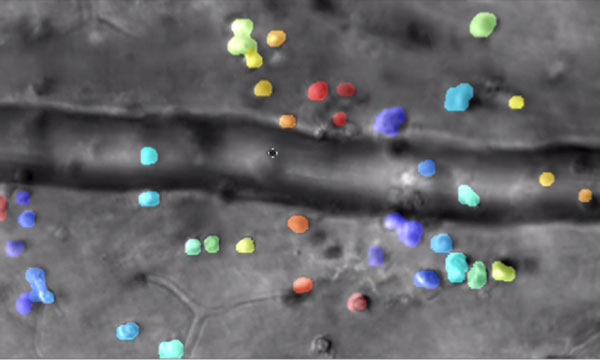
Captured by the lab of Jesse Schallek, assistant professor of ophthalmology and neuroscience, the image shows microscopic immune cells escaping a nearby blood vessel in response to inflammation. The color overlay shows computer detection of single cells that are tracked over time. (Courtesy of Schallek lab)
Rochester researchers demonstrate way to track the interactions of microscopic immune cells in a living eye without dyes or damage, a first for imaging science.
Combining infrared videography and artificial intelligence, the new technique could be a 'game-changer' for some clinical diagnoses as well as for fields like pharmaceuticals.
University of Rochester vision scientist Jesse Schallek can barely contain his excitement as he shares time-lapse videos showing immune cells moving through living retinal tissue at the back of an eye.
In one clip, immune cells crawl so slowly along the inside edge of a blood vessel that the video must be sped up 25 times to show their progress. Another cell slowly treads against the flow of blood in a vessel, like a salmon fighting its way upstream. Other immune cells leave the blood vessels and inch through the surrounding tissue, then congregate in a swarm, forming a beehive of activity.
Schallek and his vision lab at the University of Rochester Center for Visual Science and Flaum Eye Institute, have created a new microscopy technique, described in the journal eLIFE, that builds upon groundbreaking adaptive optics developed at the University more than 20 years ago.
Combined with time lapse videography and artificial intelligence software, the new technique enables researchers for the first time to noninvasively image and track—without labeling—the interactions of translucent immune cells within live retinal tissue in animals. Until now, the immune cells had to be labeled with fluorescent agents and often reinjected in order to image them—raising questions about how this might change the behavior of the cells. Another common, but limiting approach is to remove cells and study them with a microscope in a dish.
Worldwide Expert in Pediatric Ophthalmology Alex Levin Joins Flaum Eye Institute and Golisano Children’s Hospital
Monday, September 21, 2020

Internationally renowned ophthalmologist and scientist Alex V. Levin, M.D., MHSc, FRCSC, has joined the Medical Center as chief of Pediatric Ophthalmology and Ocular Genetics at the Flaum Eye Institute and chief of Pediatric Genetics at Golisano Children's Hospital. He was also named the Adeline Lutz - Steven S.T. Ching, M.D., Distinguished Professor in Ophthalmology.
Levin is the only physician in the world to simultaneously hold U.S. board certifications in Pediatrics, Ophthalmology and Child Abuse Pediatrics. He joins URMC from Wills Eye Hospital in Philadelphia.
"Dr. Levin is among the top three ophthalmologists in his field and an incredible asset to the institution," said David DiLoreto, Jr., M.D., Ph.D., chair of Ophthalmology and FEI director. "He has a collegial and inquisitive manner that inspires and engages learners at every level—from students to faculty as well as patients and their families"
Integrating clinical expertise and scientific exploration, Levin works with multispecialty teams to provide the most advanced and compassionate care for infants and children and their families. He specializes in cataracts, uveitis, glaucoma and corneal disease as well as ocular injuries from child abuse, along with ophthalmologic complications of hereditary diseases, such as retinal dystrophies and genetic syndromes in adults and children.
"Dr. Levin is one of the most distinguished ophthalmologists in the world as a clinician, researcher, and educator," said Patrick Brophy, M.D., chair of Pediatrics and Pediatrician-in-Chief for the Golisano Children's Hospital. "His innovations in studying the ocular manifestations of child abuse, as well as his vast expertise with pediatric cataract, pediatric glaucoma, and ocular genetics, will significantly advance the Medical Center's research efforts."
Joining URMC provides opportunity to take advantage of the "tremendous clinical, education and research collaborations and to work with other divisions to elevate the programs," Levin said. He will help direct creation of Ocular Genetics and Pediatric Ophthalmology fellowships and recruit trainees within the next year.
"I'm astounded by URMC's opportunities. The research at FEI is remarkable and adding ocular genetics is a great move," he said. He plans to bring FEI and GCH scientists together to strengthen research and expand horizons.
An avid reader who collects and uses antique fountain pens, Levin is a Canadian who grew up in Philadelphia, but spent most of his professional life in Toronto. He is pleased to be closer to his family and friends "back home" in Canada.
He studied at Muhlenberg College before earning his medical degree from Jefferson Medical College. He completed residencies in pediatrics at Children's Hospital of Philadelphia and then ophthalmology at Wills Eye Hospital, Sidney Kimmel Medical College. Levin then went to University of Toronto's Hospital for Sick Children for fellowship training in pediatric ophthalmology and strabismus. He later earned a Master's in Health Science in bioethics.
Funded by the National Institutes for Health, the Canadian Institute of Health, and private foundations, Levin's basic and translational research interests have included ocular genetics and gene therapy, children's vision screening, pediatric glaucoma, cataract and uveitis, ocular manifestations of child abuse and bioethics. He has published hundreds of papers and chapters, and 13 books, and lectures extensively around the world to advance understanding and treatment of eye disease and related developmental anomalies, pediatric genetics, and improve public health.
Levin's professorship is named for Lutz, a longtime patient and FEI benefactor, and her ophthalmologist Ching, who provided 20 years of expert care for her extensive retinal and corneal problems.
When Lutz died in 2011, the humble piano teacher left her life savings to support FEI research and education programs and the FEI pavilion is named for her. The professorship was established in 2014 and was originally held by Ching. When he retired, Ching's name was added to the professorship.
With Levin's recruitment, this gift continues to make a difference for the institution and its patients.
University Trustee David M. Flaum remembered as a ‘a great champion’ for University, community
Friday, August 21, 2020

University Life Trustee David M. Flaum—generous philanthropist, entrepreneur, and community advocate—passed away on August 20 at the age of 67.
"The University of Rochester and the City of Rochester have lost a great champion," said University President Sarah C. Mangelsdorf. "David Flaum built relationships as much as he built buildings, and he leaves an indelible legacy in this community and well beyond. We are saddened by David's sudden passing, but are tremendously grateful for his many lasting contributions to the University as a trustee, medical center board member, and philanthropist."
Flaum joined the University of Rochester Board of Trustees in 2007 and the Medical Center Board in 1998. During his tenure as a University board member, he served on the health affairs, facilities, and strategic and financial planning committees. He became a Life Trustee in 2017.
"In addition to supporting the institute for ophthalmology care and research that bears his name, David Flaum was extremely helpful in obtaining government funds to support construction of the Kornberg Medical Research Building, and he contributed to the growth and success of our institution in many other ways," said Mark B. Taubman, MD, CEO of URMC and dean of the School of Medicine and Dentistry. "As our entire Medical Center mourns the loss of a great champion, Lois and I have also lost a dear personal friend; we extend our deep condolences to Ilene, the Flaum family, and to David's colleagues at Flaum Management."
Rochester researcher recognized with national award for outstanding vision research
Thursday, August 20, 2020
Vision scientist David Williams is third consecutive recipient with Rochester ties.
For the third consecutive year, a member of the Rochester community has been recognized by the Association of University Professors of Ophthalmology (AUPO) for outstanding vision research.
David Williams, the William G. Allyn Professor of Medical Optics, has been selected by the association as the 2021 recipient of the RPB David F. Weeks Award for Outstanding Vision Research. The award annually recognizes and celebrates an outstanding ophthalmic vision scientist whose research has made meaningful contributions to the understanding or treatment of potentially blinding eye diseases.
The previous two recipients of the award were:
2020: Christine Curcio '81 (PhD), who is now the White-McKee Endowed Professor in Ophthalmology at the University of Alabama and director of the Age-Related Macular Degeneration Histopathology Lab.
2019: Jayakrishna Ambati '98M (Res), who is now a professor of ophthalmology at the University of Virginia.
Williams, who holds joint appointments in optics, brain and cognitive sciences, ophthalmology, and biomedical engineering, is widely regarded as one of the world's leading experts on human vision. As a pioneer in using new technologies that improve the eyesight of people around the world, he and his research team demonstrated the first adaptive optics system for the eye, making it possible to image individual retinal cells. The techniques developed by Williams and his group have also improved vision in patients with contact lenses, intraocular lenses, and laser refractive surgery. For example, the methods Williams's group developed are used in many of the Lasik procedures conducted worldwide today.
Williams additionally serves as director of the Center for Visual Science, a research program consisting of more than 37 faculty members from seven different departments dedicated to understanding how humans see, as well as the disorders that compromise sight.
Williams joined the Rochester faculty in 1981, and served as dean for research in Arts, Sciences & Engineering from 2011 to 2019. He is a fellow of the Association for Research in Vision and Ophthalmology, the Optical Society of America, and the American Association for the Advancement of Science. In 2017, he was named a member of the National Academy of Sciences.
The Weeks Award is scheduled to be presented to Williams at the AUPO Annual Meeting in February 2021.
‘Time is vision’ after a stroke
Wednesday, May 27, 2020

A research team including professor of ophthalmology Krystel Huxlin (right, in a 2019 photo) provided stroke patients with a form of physical therapy for the visual system using a device Huxlin developed. (University of Rochester photo / J. Adam Fenster)
A person who has a stroke that causes vision loss is often told there is nothing they can do to improve or regain the vision they have lost.
But research from the University of Rochester,published in the journal Brain, may offer hope to stroke patients in regaining vision.
The Rochester team found that survivors of occipital strokes—strokes that occur in the occipital lobe of the brain and affect the ability to see—may retain some visual capabilities immediately after the stroke, but these abilities diminish and eventually disappear permanently after approximately six months. By capitalizing on this initial preserved vision, early vision training interventions can help stroke patients recover more of their vision loss than if training is administered after six months.
"One of our key findings, which has never been reported before, is that an occipital stroke that damages the visual cortex causes gradual degeneration of visual structures all the way back to the eyes," says Krystel Huxlin, the James V. Aquavella, MD Professor in Ophthalmology at the University of Rochester's Flaum Eye Institute.
The Rochester research team—including Elizabeth Saionz, a PhD candidate in Huxlin's lab and the first author of the paper; Duje Tadin, professor and chair of the Department of Brain and Cognitive Sciences; and Michael Melnick, a postdoctoral associate in Tadin and Huxlin's labs—also discovered that early intervention in the form of visual training appears to stop the gradual loss of visual processing that stroke victims may experience.
Vision stroke rehabilitation remains a developing field, and previous studies and trials of experimental therapies have focused on patients with chronic vision loss—that is, patients who are more than six months post-stroke.
"Right now, the 'standard of care' for vision stroke patients is that they don't receive any targeted therapy to restore vision," Saionz says. "They might be offered therapy to help maximize use of their remaining vision or learn how to navigate the world with their new limited vision, but there are no treatments offered that can give them back any of the vision that they lost."
The new study compared chronic patients—those who were more than six-months post-stroke—with early subacute patients, who started training within the first three months after their stroke.
The researchers trained both groups of stroke patients using a computer-based device Huxlin developed. The training is a form of physical therapy for the visual system and involves a set of exercises that stimulates undamaged portions of the visual cortical system to use visual information. With repeated stimulation, these undamaged parts of the brain can learn to more effectively process visual information that is not filtered by the damaged primary visual cortex, partially restoring conscious visual sensations.
The researchers discovered that the subacute patients who underwent such vision training recovered global motion discrimination—the ability to determine the direction of motion in a noisy environment—as well as luminance detection—the ability to detect a spot of light—faster and much more efficiently than the chronic patients.
Overall, the group's findings suggest that individuals may maintain visual abilities early after a stroke, indicating they have preserved some sensory information processing that may temporarily circumvent the permanently damaged regions of the brain. Early visual training may therefore be critical both to prevent vision from degrading and to enhance restoration of any preserved perceptual abilities.
"For the first time, we can now conclusively say that just as for sensorimotor stroke, 'time is vision' after an occipital stroke," Huxlin says.
The study was funded by the National Institutes of Health, including NIH's National Center for Advancing Translational Sciences and National Institute of General Medical Sciences, as well as the Research to Prevent Blindness Foundation.
Mina Chung, Retinal Surgeon and Researcher, Dies at 51
Monday, February 17, 2020

Mina Millicent Chung, M.D., an ophthalmologist and retina specialist who helped blind children to see and furthered the study of retinal disease, including macular degeneration, died Feb. 13 after a fall while skiing in Cortina d'Ampezzo, Dolomites, Italy. She was 51.
Chung was an associate professor of ophthalmology at URMC's Flaum Eye Institute and a faculty member in the University's Center for Visual Science. Before being recruited to Rochester in 2002, she completed a fellowship in vitreoretinal surgery at the University of Iowa College of Medicine, following residency and postdoctoral research at USC University Hospital in Los Angeles, where she served as chief resident from 2000 to 2002. Chung was a 1994 graduate of the Yale University School of Medicine who received her undergraduate degree from Yale in 1990.
As a clinician, Dr. Chung provided medical and surgical care to patients of all ages suffering from retinal diseases such as age-related macular degeneration, diabetic eye disease, genetic retinal diseases, ocular trauma, uveitis and other diseases relating to the back of the eye. She was a key member of Flaum Eye Institute's pediatric artificial corneal transplant team and a specialist in pediatric retinal surgeries.
"Mina Chung was an exceptionally skilled, caring surgeon who also excelled as a scientist and educator in the field of ophthalmology," said Mark B. Taubman, M.D., president and CEO of the University of Rochester Medical Center. "She was a valued member of our faculty who will be missed by the many patients and colleagues whose lives she touched, not just here in Rochester but around the world."
David A. DiLoreto, M.D., Ph.D., Chair of Ophthalmology and Director of the Flaum Institute, also praised Chung for her dedication to patients. "Mina was one of the most dedicated and hardworking physicians I have ever known," DiLoreto said. "Mina did whatever was needed to serve her patients, and she did it with a smile and enthusiasm that was infectious to all of us who had the privilege of working with her."
Dr. Chung's research interests included inherited retinal diseases and genetic factors contributing to age-related macular degeneration. As part of the University's Advanced Retinal Imaging Alliance (ARIA), she specialized in developing optics technologies to study early cellular changes in macular diseases.