Bone Health: What’s Menopause Got to Do with It?
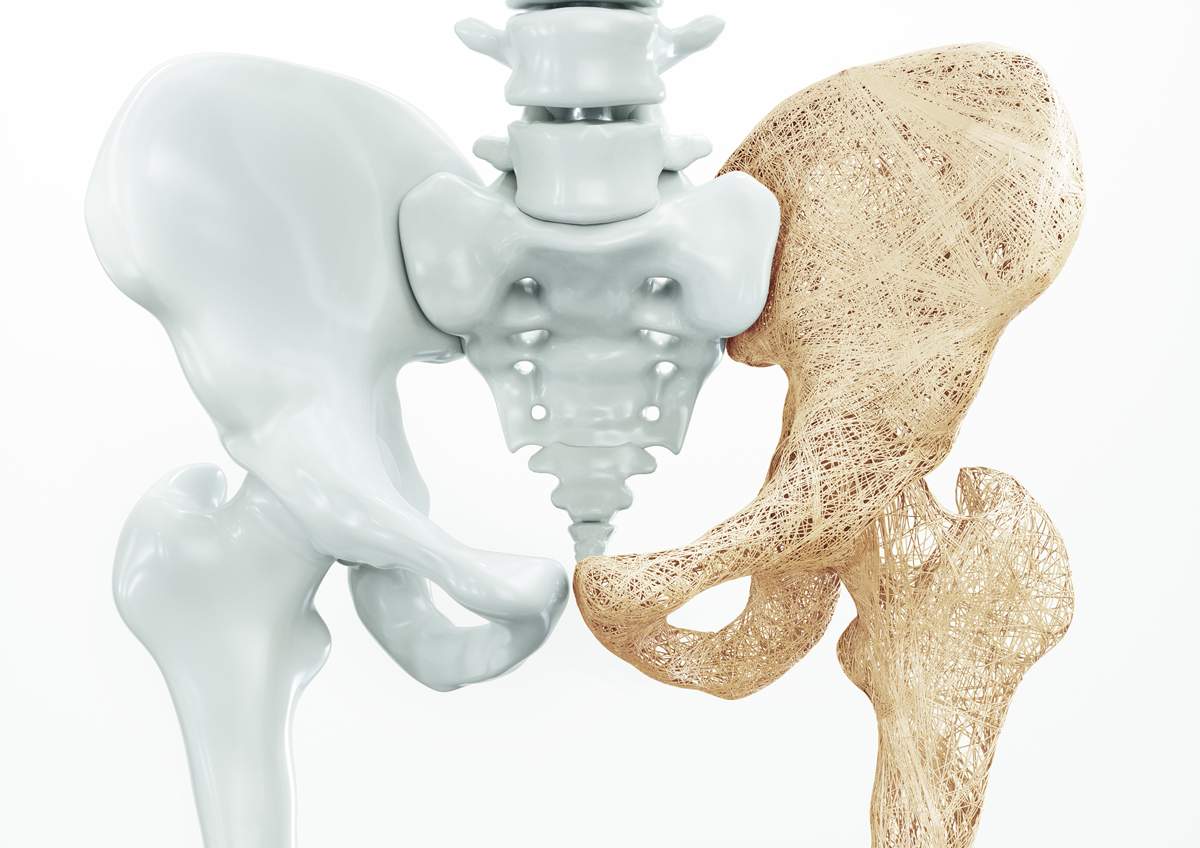
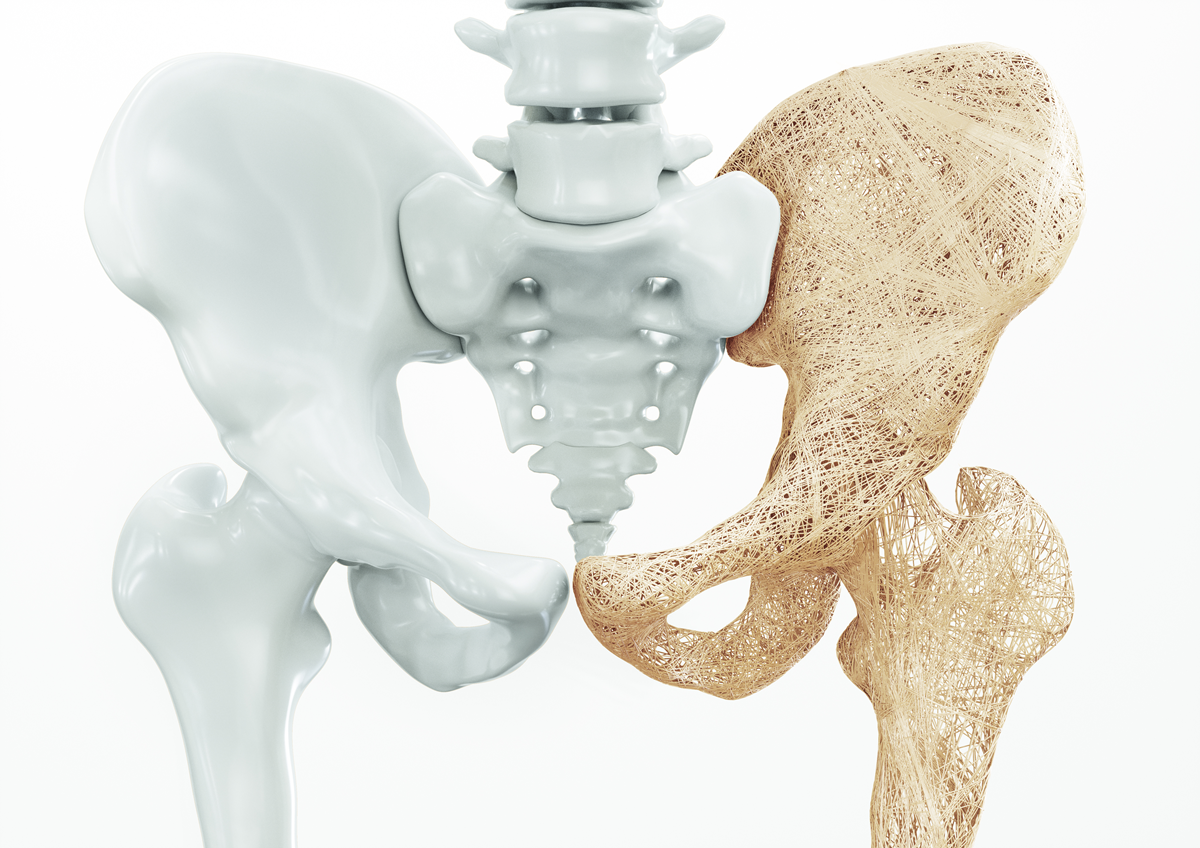
You may be unaware that your bones are engaging in a balanced, continuous process of remodeling; laying down new bone while eliminating old bone. So why is this process jeopardized in menopause?
Bone is produced by osteoblasts. These cells lay down a material called osteoid, composed of a collagen in a lattice frame, and fill it in with inorganic material called hydroxyapatite, a complex molecule of calcium and phosphate written as Ca10(PO4)6(OH)2. Hydroxyapatite gives bone its strength and resiliency, and since it contains 99% of the body’s calcium, it serves as the main reservoir when calcium is needed for other bodily processes.
Bone is broken down by osteoclasts, which are derived from stem cells in the blood. Osteoclasts are activated by a group of inflammatory cytokines that stimulate osteoclast activity. When osteoclasts attach to bone matrix, their edges release acid and other substances to dissolve hydroxyapatite, thus releasing calcium, other minerals, and protein materials into the blood and then urine.
Bone turnover is regulated by several factors. Hydroxyapatite requires the availability of calcium which is regulated by vitamin D. Vitamin D3 (called calciferol) is synthetized in the skin by ultraviolet B light. Vitamin D2 is produced by dietary plants. Both are converted in the liver to 1,25 dihydroxy vitamin D, which controls calcium absorption in the small intestine. Parathyroid hormone (PTH) has little effect on intestinal calcium absorption but stimulates osteoblast activity and promotes calcium reabsorption in the kidney.
Bone strength changes over the lifetime. Peak bone strength occurs between the ages of 20 to 30. During menopause, bone loss accelerates in the three years before and the three years after the final menstrual period at a rate of 2% per year, then slows to 1% a year afterward.
Bone health is measured by Bone Mineral Density (BMD), determined by Dual Energy X‐Ray Absorptiometry (DXA Scan). By this technique, two X‐ray beams of different energy are aimed at bone. The results, presented as a T Score, are compared to that of the average race‐matched young normal female. Measurements of ‐1 to ‐2.5 Standard Deviations (SD) below peak normal values of the lumbar spine, or femur neck (hip) reflect low bone density (osteopenia) and ‐2.5 SD or greater reflect significant bone loss (osteoporosis). For white women over 50 years, 13% to 18% have osteoporosis of the hip, and 30% to 50% have osteopenia. By age 80, over 50% are likely to exhibit osteoporosis, making hip fractures, with a 25% mortality rate in the first year, a serious risk.
Age, a family history of osteoporosis, smoking, malnutrition, low estrogen levels, and chronic disease are all risk factors for bone loss. Because natural estradiol inhibits cytokine‐induced osteoclast activity, the expected decline of estradiol in menopause contributes to the risk of osteoporosis. Current daily recommendations for menopausal women who are not on estrogen therapy are 1200 to 1500 mg calcium and 800 IU of vitamin D. Other preventive measures include weight‐bearing exercises, fall prevention strategies like Tai Chi, and hormone therapy that includes estrogen. All can decrease a woman’s risk
of bone loss.
By James Woods, M.D.
Dr. Woods treats patients for menopause at the Hess/Woods Gynecology Practice.
Disclaimer: The information included on this site is for general educational purposes only. It is neither intended nor implied to be a substitute for or form of patient specific medical advice and cannot be used for clinical management of specific patients. Our responses to questions submitted are based solely on information provided by the submitting institution. No information has been obtained from any actual patient, and no physician‐patient relationship is intended or implied by our response. This site is for general information purposes only. Practitioners seeking guidance regarding the management of any actual patient should consult with another practitioner willing and able to provide patient specific advice. Our response should also not be relied upon for legal defense, and does not imply any agreement on our part to act in a legal defense capacity.
James Woods | 2/2/2015